Ciencia y Salud, Vol. VI, No. 2, mayo-agosto, 2022 • ISSN (impreso): 2613-8816 • ISSN (en línea): 2613-8824 • Sitio web: https://revistas.intec.edu.do/
KNOWLEDGE, PERCEPTIONS, NEEDS AND CHALLENGES OF DOMINICAN ADOLESCENTS WITH TYPE 1 DIABETES MELLITUS
Conocimientos, percepciones, necesidades y desafíos de los adolescentes dominicanos con diabetes mellitus tipo 1
Cómo citar: Moore de Peralta A, Cepeda J, Abreu Rodríguez G. Knowledge, Perceptions, Needs and Challenges of Dominican Adolescents with Type 1 Diabetes Mellitus. cysa [Internet]. [citado 17 de mayo de 2022];6(2):23-3. Disponible en: https://revistas.intec.edu.do/index.php/cisa/article/view/2504
Acknowledgment
This study was developed with funds from the National Fund for Innovation and Scientific and Technological Development [Fondo Nacional de Innovación y Desarrollo Científico y Tecnológico] (FONDOCyT), administered by the Ministry of Higher Education, Science and Technology [Ministerio de Educación Superior, Ciencia y Tecnología] (MESCyT). The research project was managed by the Institute of Tropical Medicine and Global Health [Instituto de Medicina Tropical y Salud Global] (IMTSAG) of the Iberoamerican University [Universidad Iberoamericana] (UNIBE). The research team would like to thank all study participants for their contributions, and the pediatric endocrinology team at the Learning to Live Foundation for supporting the recruitment process for this study.
Introduction
In the Dominican Republic (D. R.), chronic diseases are among the top 10 causes of death, with diabetes ranked among the top four causes of death1. Type 1 Diabetes Mellitus (T1DM) is an autoimmune disease that requires lifelong insulin replacement therapy to avoid future complications2. The International Diabetes Federation (IDF) estimates that 121,400 children and adolescents had T1DM at the North American and Caribbean region level in 20193. The complications of DMT1 have increased in D. R., impacting medical expenses, affecting the quality of life of patients, and increasing morbidity and mortality due to this disease4,5. The D. R. has a robust health system in which many communicable diseases are under epidemiological surveillance and are monitored at the national level. However, there are currently no mechanisms to measure, monitor and address chronic noncommunicable diseases6. Therefore, it is difficult for health center staff to monitor the progress of T1DM in their patients, who require constant and permanent treatment2.
Studies have shown that adolescence is a stage in which metabolic control becomes more complex due to hormonal changes related to puberty and that are associated with insulin resistance7, and also because young people begin to detach the management of their disease from the control assumed by their parents during childhood8, 9. However, successful self-management of the disease requires motivation, knowledge, and patient empowerment, which influences glycosylated hemoglobin (HbA1c) levels10. The self-management of T1DM has evolved to require patients to have the ability to formulate algorithms for insulin treatment based on the combination of interactive physiological parameters for the control of postprandial blood glucose levels11, 12, 13, 14. For instance, therapeutic education can help patients with T1DM in the self-management of their disease15, 16.
The purpose of this study was to determine the level of knowledge, perceptions, needs and challenges of Dominican adolescents with T1DM through a qualitative study and using the Health Belief Model (HBM) as a conceptual framework17. Previous studies have designed scales based on HBM dimensions to determine the extent to which the beliefs and perceptions of patients with T1DM influence the self-management of their disease18-20. The research questions that guided this study were: (1) What is the level of knowledge about T1DM and perceptions about self-management of Dominican adolescents suffering from this disease? and (2) What are the needs and challenges reported by Dominican adolescents for T1DM’ self-management? The objective of this study was to guide the development of a mobile application to assist Dominican adolescents in self-managing their condition, and to reduce T1DM complications.
Methodology
Descriptive and qualitative study, based on telephone interviews with 23 adolescents between 14 and 18 years old, of both sexes and any marital status, who suffered from T1DM. Participants were selected through convenience, not probabilistic, sampling, using a list of patients provided by the Learning to Live Foundation (Fundación Aprendiendo a Vivir). The exclusion criteria included severe T1DM (e.g., severe complications and disability [amputations, blindness, deafness], frequent hospitalizations [e.g., at least 6 times a year], etc.). The sample consisted of 23 Dominican adolescents (100%), predominantly male (61%), students (83%) and more than one year after being diagnosed with DMT1 (61%).
Instruments
All the instruments used in the study were approved by the Ethics Committee of the Universidad Iberoamericana (UNIBE). Interviews were conducted using a structured guide with open-ended questions. This guide was prepared by the research team based on a review of the literature. The guide contained 17 questions and was piloted by diabetes specialists.
Data collection
Participants (i.e., the teens and their parents or guardians) were previously contacted by phone to ask them to participate in the study. A convenient date and time were agreed with those parents or guardians and adolescents who agreed to participate by signing a consent form that included contact information for the principal investigators. In addition, participants were informed in the consent about their right not to answer questions they considered inappropriate or sensitive; as well as their right to leave the study if they did not wish to continue participating. The interviews lasted on average between 40 to 60 minutes.
Data analysis
The analysis was performed using the qualitative data analysis program NVivo, and through a deductive approach to list the needs, perceptions, and challenges reported by the participants; as well as an inductive approach to identify aspects that were not anticipated by the research team.
Results
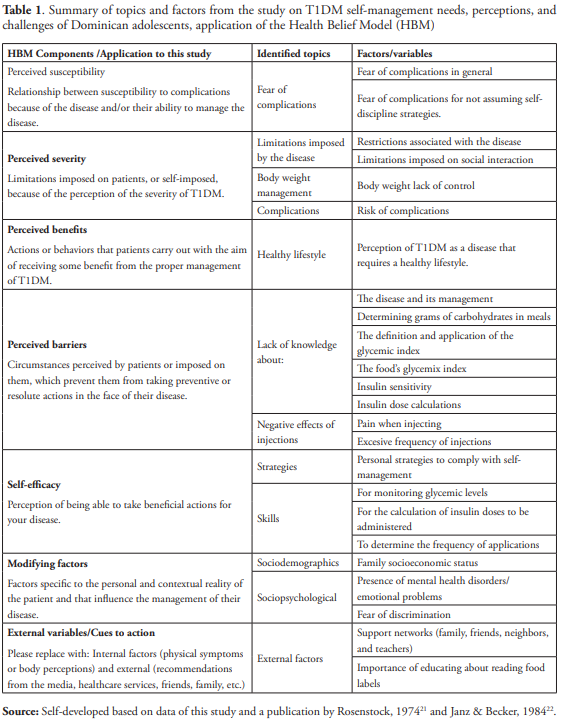
The results section was organized based on the HBM components, which included perceived susceptibility and severity, perceived barriers and benefits, self-efficacy, and modifying factors17. Table 1 includes a summary of the topics and factors that were identified during the data analysis, organized according to the HBM.
Perceived susceptibility
In relation to participants’ perceived susceptibility, a fear of complications was identified. One patient referred to living in fear of having complications associated with diabetes. Some participants reported aspects related to the perceived susceptibility of having problems or complications due to not assuming self-discipline strategies to comply with the schedules designated by their doctor for the administration of insulin. An example of this was what one of the participants who said, “... I am always attentive to that, I think, well... if I don’t put it on [insulin] I’ll have problems”.
Perceived severity
Regarding the limitations imposed on patients, or self-imposed, because of the perception of T1DM severity, two participants described diabetes as a health condition and a disease without a cure.
Severity related to limitations or restrictions that patients associate with the disease
About six participants, upon hearing the word diabetes, thought about limitations in food intake, “[a] person who can’t eat a lot of sugar or who is self-conscious about not eating certain things”. According to eleven participants, after their diagnosis of T1DM, they have had to give up foods that were to their liking, such as sweets, soft drinks, etc. They said that, as teenagers, they have a greater affinity for “junk foods” and have a hard time having to control the desire to eat them. Some understand that the disease has led them to having a healthier life, while others struggle with the anxiety of not being able to eat the same as before, or the same as the people around them eat.
Severity related to disease-imposed limitations on social interaction
Regarding changes related with social interactions, participants expressed that due to T1DM they must restrict themselves from certain meals when they meet at certain social events. One participant said, “[m]ust have some degree of control on what I eat when going out with my friends, like popcorn, or a certain amount of food...”.
Lack of body weight’s control
Another effect that was mentioned by the participants was the change in their body weight, commenting that, if they did not maintain good control of their disease, it was difficult for them to maintain a stable weight. Regarding that, one participant said, “... at first, it wasn’t easy for me because I was chubby... since I developed the disease, I got skinny...”.
Perceived benefits
Perceived benefits included the perception of T1DM as a healthy lifestyle, or as a disease that requires a healthy lifestyle. A group of participants saw the regimen that a person with diabetes should followed as an advantage, as it forces them to lead a life focused on health, something that is beneficial for anyone, regardless of whether they have diabetes. One participant said, “... but diabetes actually if you know or learn how to take it is not so difficult and is not carried as a disease, but as a way of living...”. A group of six participants agreed that T1DM can be defined as a life or health condition that leads to a healthy lifestyle.
Perceived barriers
Among the barriers identified are the lack of knowledge about the disease and its proper management, the determination of grams of macronutrients from meals, the definition and familiarization with the glycemic index, the definition of insulin sensitivity, and insulin dose calculations. In addition, pain and frequency of injections were identified as barriers.
Lack of knowledge
Participants’ level of knowledge was deficient in topics related to the definition of diabetes, up to topics such as insulin sensitivity. Also, little management was demonstrated in the understanding of the glycemic index, the definition, and types of insulin, as well as in everything related to the calculation of the insulin dose.
DMT1 Definition and conceptualization
Participants were asked what the first thing they thought of when they heard the word diabetes. Participants’ responses reflected lack of knowledge about what T1DM is and how it occurs. Two participants referred to the disease as the presence of sugar or elevated levels of it in the blood. In that sense one participant said, “[w]ell when I hear the word diabetes, that means there is sugar in the blood”. Two participants referred to insulin deficiency as a cause of diabetes, one of them said, “[w]ell, when I hear the word diabetes what comes to mind ..., it is a condition that I have as if I do not produce insulin or that I lack insulin”. To analyze the participants’ level of knowledge, they were also asked to define T1DM in their own words. Their responses were classified as giving a moderately oriented definition and a non-oriented definition. In relation to the moderately oriented definition of T1DM, this disease was defined by three participants as diabetes where the pancreas does not produce insulin or as a person itself, whose pancreas does not possess insulin. Four participants defined the disease as “any disease”, which was given to them, without mentioning details that differentiate it from another disease. Three other participants gave their definition expressing that DMT1 is a disease diagnosed in minors or with which one is born.
Determination of grams of carbohydrates from meals
Twenty-two participants expressed that they were not able to determine the grams of carbohydrates from the foods they eat. Of this group, most directly admitted that they did not know or did not understand how to determine this, while the others tried to explain this procedure erroneously.
Glycemic index definition and level of familiarization with the food’s glycemic index
Many participants directly expressed that they were unaware of the glycemic index, and others mistakenly understood that the glycemic index referred to the amount of glucose and/or fat in a food. In relation to this it was said, “I guess that it is the amount of sugar or fat it contains”. Some admitted that they had never heard of it. Even after the interviewer explaining the concept to the participants, a group of nine participants said they were unable to give an answer to the question. Others linked the definition of glycemic index to intuitively identifying a food high in carbohydrates, fats or whether it is sweet, and categorizing it as a food that will potentially increase their glycemia.
Definition of insulin sensitivity
Participants were far from the true definition of insulin sensitivity and tried to relate this concept to different variables of the same disease. One of these variables was insulin, which was related as an impossibility of administering it due to some damage that it could produce. A participant said: “[t]hat he is sensitive... like it could hurt me, I don’t know if I’m okay, like insulin causing me an allergy or something like that”. A group of sixteen participants admitted directly that they did not know the concept. One participant said “[i]nsulin sensitivity... I’ve never heard of that”.
Insulin dose calculation
We asked participants to explain the calculation they perform to know the dose of insulin to be administered to themselves. All participants admitted not to perform any calculations and to be unfamiliar with its importance. One participant reported having an insulin pump, which does this whole process automatically, and said “[r]eally it’s calculated by a sugar machine I have on, you put the carbs on it, and it does the math”.
Pain and frequency of injections
The constant frequency of injections that these patients must undergo is very high and seems to cause in many patients some demotivation to comply with their management. Some participants reported that it is a bit tedious to have to inject daily. One of the participants said he decided to stop the monitoring, as he has a lot of pain in his fingers.
Self-efficacy
Participants identified several strategies when asked about aspects of managing their disease and how they execute it.
Personal strategies for T1DM self-management’s compliance
Many of the participants reported that one of the strategies they use most is to keep a fixed schedule and to comply with it, so that it becomes a habit and makes it more difficult to fail. Participants seem to be very committed to meeting their schedules. One of the participants explained what he does to maintain that commitment, “... in the morning I don’t wake up late... directly from the moment I get up I go and put it on; and in the afternoon I put it on before half past six”. A group of participants reported that they are simply aware of their responsibility all the time, since they are aware of the consequences of not doing so.
Glycemic levels’ monitoring
Many participants agreed about using the glucometer to assess their blood glucose levels. Many of them reported doing it themselves, and a few mentioned been assisted by their relatives. Seventeen of the participants reported performing the monitoring daily, either with each meal or every two to three hours. Six participants mentioned that the frequency of monitoring their blood glucose depends on whether they feel any symptoms of hyperglycemia or hypoglycemia, dizziness, headache, etc.
Calculation of insulin dose to be administered and frequency of application
Knowledge of the insulin dose calculation is a determining factor for the success of glycemic control in people with diabetes. Most participants reported having a fixed dose of insulin designated by their doctor, which they intuitively modify in case of hyperglycemia or hypoglycemia.
Modifying factors (sociodemographic, structural, sociopsychological, level of knowledge and acquired skills)
Among the modifying factors we identified the socioeconomic level of the family, the presence of mental health disorders and emotional problems, and the fear of discrimination.
Socioeconomic status of the family
The influence of the family’s economic capacity was evident in three participants who reported as important the fact that their family can cover the expenses of managing their disease. A participant said, “... I must be grateful because, thanks God, I have a family that can cover the expenses that this disease entails ..., it is a bit expensive”.
Mental health/emotional disorders
Anxiety was a recurring theme mentioned by the participants. They mentioned how tedious it becomes for them to manage the disease when they are experiencing emotional instability. In this regard, one participant said: “[A]lso I have had already experienced many issues because... I am a patient who suffers a lot of anxiety and then sometimes I have eaten one or another sweet...”. Another aspect mentioned by the participants was the fluctuation in their sugar levels and its influence on their mood swings.
Fear of discrimination
Regarding the changes in the social aspect, participants commented on how some people prefer not to approach them due to their illness. One participant said “... problems I’ve had with people, you know, to always have me on the side and that”.
External variables or cues to action (Media, health campaigns, peer, or support groups)
The main support expressed by participants comes from their family. According to 23 of the participants, family plays a vital role in the management of their disease. Whether it’s to remind them of the administration of their medications, or to help them make better decisions in their diet, also, for the monitoring of their glycemia and as an emotional support. As immediate family, parents and siblings were frequently mentioned. Some participants said that friends and classmates also often support them in deciding what foods they can consume or simply to be present in case something happens to them. There were also two participants who said they rely on their neighbors and their school’s teachers. Health professionals were also mentioned by two participants: both doctors and nurses of their academic campus.
Discussion
The HBM17 was used by the research team, in the data analysis phase, to organize the identified determinants that influence the health behaviors of adolescents with T1DM. One of the most reported fears by the participants in relation to their perceived susceptibility was the fear of complications, mainly those complications related to the fact of not assuming self-discipline related strategies. Studies have shown the importance of continuous support and motivation to facilitate T1DM proper management and complications’ reduction10,18. Regarding perceived severity, some of the participants referred to T1DM as a disease “without a cure”, reflecting a fatalistic attitude23 that visualizes the medical-clinical consequences of the disease as terminal. Previous studies found that within the perceived severity some of the complications reported by adolescents with T1DM included ketoacidosis, blurred vision, kidney damage and neuropathies18.
Among the reported benefits, many of the participants referred to the disease as something that forces them to lead a healthy life, and which becomes a “way of life”. These findings are consistent with what has been found in previous studies18. In our study, participants visualized how suffering from the disease would promote the perceived benefits of maintaining a healthy life; but at the same time pointing out the importance of having the necessary resources to be able to maintain a healthy lifestyle that is suitable for the disease through healthy eating and an active life24, which reflects the relevance of the social determinants of health in the proper management of the disease.
Considering the limited capacity of the Dominican Republic’s public health system to provide tools and continued support to patients for self-managing chronic diseases6, it is important that therapeutic education strategies15 also focus on increasing the level of self-efficacy of adolescents with T1DM. The socioeconomic status of the family was identified by several participants as a relevant determinant to be able to manage such an “expensive” disease. Other determinants mentioned at the individual level included the patient’s attitude towards living with the disease, the presence of emotional disorders or mental health problems that can make it more difficult to manage the disease and living in fear of discrimination by people who do not know the disease well. Previous studies have shown the need for accessible interventions (e.g., internet training, mobile applications, etc.) to help adolescents and their families cope with the stress related to T1DM and to increase their self-efficacy7.
The external variables identified that could facilitate the self-management of the disease included the existence of support networks represented by family, friends, neighbors, and teachers. Some participants reported that one of the aspects in which the family25 helps them a lot is in the fulfillment of the schedule for insulin administration. However, other studies have also revealed a potential conflict with the involvement of parents in the development of adolescents’ sense of self-determination26, 27. The present study was not without limitations. Our results did not allow us to generalize the results to the entire population of Dominican adolescents with T1DM. However, having selected patients in a health facility that primarily cares for patients from low- and middle-income families would help us gain insight into the situation of patients who face the greatest potential challenges in managing their disease due to their socioeconomic status. It is possible that participants’ self-report on their situation could be biased by “social desirability”28. Conducting the interviews by telephone may have helped reducing this bias.
Conclusions and recommendations
The transition to adolescence in young people with T1DM is a period of many challenges both at the level of development, physiologically and in their behavior7, 8. There is a great need for culturally relevant interventions to improve metabolic control and psychosocial aspects in adolescents with T1DM29. Incorporating affected adolescents’ perspectives, contextual realities, and knowledge about the disease and its management could influence the development of culturally appropriate interventions. Our findings reflected the relevance of applying holistic and multilevel approaches, as the HBM17, to the study of and intervention design for T1DM self-management. Longitudinal studies could assist in exploring developmental changes in adolescents’ T1DM self-management and related determinants. In addition, future studies should incorporate the perspectives of parents in conjunction with that of adolescents with T1DM, to generate a more holistic and comprehensive view of the situation and challenges faced by these patients.
Referencias
- World Health Organization [Internet]. Ginebra: c2021. Informe mundial sobre la Diabetes. WHO Document Production Services; 2016 [citado 25 febrero 2021]. Disponible en: https://apps.who.int/iris/bitstream/handle/10665/254649/9789243565255-spa.pdf;jsessionid=AF0D1391B3097878F23AAE6793E7F581?sequence=1
- Calderón C, Carrete L, Vera J. Validación de una escala de creencias de salud sobre diabetes tipo 1 para el contexto mexicano: HBM-T1DM. Salud Pública Mex. 2018; 60:175-183. Disponible en: https://doi.org/10.21149/8838
- International Diabetes Federation. Atlas de la Diabetes de la FID [Internet]. Inís Communication; 2019 [citado 25 febrero 2021]. Disponible en: https://www.diabetesatlas.org/upload/resources/material/20200302_133352_2406-IDF-ATLAS-SPAN-BOOK.pdf.
- Organización Mundial de la Salud [Internet]. Informe mundial sobre la diabetes. Geneva: OMS; 2016. Disponible en: http://www.who.int/diabetes/global-report/es/
- Pichardo R, Gonzalez AR, Escaño F, Rodríguez C, Jiménez RO. Estudio de los factores de riesgo cardiovascular y síndrome metabólico en la República Dominicana (EFRICARD II). Revista Archivos Dominicanos de Cardiología. 2012, Edición especial. Disponible en: https://static.elsevier.es/cardio/static/premio_cardio/revista-dominicana-cardiologia.pdf.
- WHO and UN Partners [Internet]. Country statistics and global health estimates. 2015. Disponible en: http://who.int/gho/mortality_burden_disease/en/
- Whittemore R et al. An internet coping skills training program for youth with type 1 diabetes: six-month outcomes. Nurs Res. 2012; 61(6): 395-404. Disponible en: doi: https://doi.org/10.1097/NNR.0b013e3182690a29.
- Ellis DA, Podolski C-L, Frey M, Naar-King S, Wang B, Moltz K. The role of parental monitoring in adolescent health outcomes: Impact on regimen adherence in youth with type 1 diabetes. J Pediatr Psychol. 2007; 32(8):907-7. Disponible en: https://doi.org/10.1093/jpepsy/jsm009
- Nathan DM, Bayless M, Cleary P, Genuth S, Gubitosi-Klug R, Lachin JM, Lorenzi G, Zinman B; DCCT/EDIC Research Group. Diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: advances and contributions. Diabetes. 2013 Dec; 62(12):3976-86. Disponible en https://doi.org/10.2337/db13-1093
- Casey D, Murphy K, Lawton J, White FF, Dineen S. A longitudinal qualitative study examining the factors impacting on the ability of persons with T1DM to assimilate the Dose Adjustment for Normal Eating (DAFNE) principles into daily living and how these factors change over time. BMC Public Health. 2011; 11(1):672. Do1: https://doi.org/10.1186/1471-2458-11-672
- Grant L, Lawton J, Hopkins D, Elliott J, Lucas S, Clark M et al. Type 1 diabetes structured education: What are the core self-management behaviours? Diabet Med. 2013; 30(6):724-30. DOI: https://doi.org/10.1111/dme.12164
- Lopes Souto D, Lopes Rosado E. Use of carb counting in the dietary treatment of diabetes mellitus. Nutr Hosp. 2010; 25:18-25.
- Dias VM, Pandini JA, Nunes RR, Sperandei SL, Portella ES, Cobas RA et al. Effect of the carbohydrate counting method on glycemic control in patients with type 1 diabetes. Diabetol Metab Syndr. 2010 Aug 17; 2:54. DOI: 10.1186/1758-5996-2-54
- Son O, Efe B, Erenoğlu Son N, Akalin A, Kebapçi N. Investigation on Carbohydrate Counting Method in Type 1 Diabetic Patients. BioMed Research International. 2014; Disponible en: https://doi.org/10.1155/2014/176564
- World Health Organization. Therapeutic patient education. Continuing education programmes for health care providers in the field of prevention of chronic diseases. Copenhagen: World Health Organization Regional Office for Europe; 1998. Disponible en: https://apps.who.int/iris/handle/10665/108151
- Wiley J, Westbrook M, Long J, Greenfield JR, Day RO, Braithwaite J. Diabetes education: the experiences of young adults with type 1 diabetes. Diabetes Ther. 2014;5(1):299-321. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4065294/
- Champion VL, Skinner CS. The Health Belief Model. In: Glanz K, Rimer BK, K. V, eds. Health Behaviour and Health Education Theory, Research, and Practice. 4th Edition. San Francisco: John Wiley & Sons, Inc. 2008; 45-65.
- Calderón C, Lorena C, Vera J. Validación de una escala de creencias de salud sobre diabetes tipo 1 para el contexto mexicano: HBM-T1DM. Salud pública Méx [serial on the Internet]. 2018 Apr; 60(2):175-83. Disponible en: https://doi.org/10.21149/8838
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15(2):175-83.
- Bandura A. Guide for constructing self-efficacy scales. In: Self-efficacy beliefs of adolescents. Greenwich, CT, Estados Unidos de América: Information Age Publishing. 2006;307-77.
- Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974; 2(4): 328-35.
- Janz NK, Becker MH. The Health Belief Model: A decade later. Health Educ Q. 1984; 11(1):1-47.
- Abraído-Lanza AE, Viladrich A, Flórez KR, Céspedes A, Aguirre AN, De La Cruz AA. Commentary: fatalismo reconsidered: a cautionary note for health-related research and practice with Latino populations. Ethn Dis. 2007; 17(1):153-8.
- Caplan S, Sosa Lovera A, Reyna Liberato P. A feasibility study of a mental health mobile app in the Dominican Republic: The untold story. Int J Ment Health. 2018; 47(4):311-45. Disponible en https://doi.org/10.1080/00207411.2018.1553486
- Marín G, VanOss Marín B. Research with Hispanic populations. California: SAGE Publications, Inc.; 1991. Disponible en: https://dx.doi.org/10.4135/9781412985734
- Coupey SM, Cohen MI. Special considerations for the health care of adolescents with chronic illnesses. Pediatr Clin North Am. 1984; 31(1):211-9. Disponible en https://doi.org/10. 1016/s0031-3955(16)34547-3
- Weinger K, O’Donnell KA, Ritholz MD. Adolescent views of diabetes-related parent conflict and support: a focus group analysis. J Adolesc Health. 2001; 29(5):330-6. Doi: https://doi.org/10.1016/s1054-139x(01)00270-1.
- Arredondo EM, Pollak K, Costanzo PR. Evaluating a stage model in predicting monolingual Spanish-speaking Latinas’ cervical cancer screening practices: the role of psychosocial and cultural predictors. Health Educ Behav. 2008; 35(6):791-805. Doi: 10.1177/10901981073 03250.
- Guo J, Whittemore R, Grey M, Wang J, Zhou Z-G, He G-P. Diabetes self-management, depressive symptoms, quality of life and metabolic control in youth with type 1 diabetes in China. J Clin Nurs. 2013; 22(1-2):69-79. DOI: https://doi.org/10.1111/j.1365-2702.2012.04299.x

