Ciencia y Salud, Vol. 9, No. 3, septiembre-diciembre, 2025 • ISSN (impreso): 2613-8816 • ISSN (en línea): 2613-8824
MODIFIABLE FACTORS AND DETERMINANTS ASSOCIATED WITH POOR LIPID CONTROL IN INDIVIDUALS WITH HIGH CARDIOVASCULAR RISK
Factores modificables y determinantes asociados un mal control lipídico en individuos con alto riesgo cardiovascular
DOI: https://doi.org/10.22206/cisa.2025.v9i3.3228
Jenny L. Cepeda-Marte1, Ricardo E. Hernández-Landa2, Carlos Ruiz-Matuk3, Marc B. Bello-Figueroa4, Kristy Polanco5, Daniela Salado6, Valery Carrion7, Jazmin Pantaleon Vásquez8, Pedro Vargas Bocio9, Roberto Garcia10, Elizabeth Sánchez Almánzar11
Recibido: 09/06/2024 ● Aceptado: 21/02/2025
Cómo citar: Cepeda-Marte, J. L., Hernández-Landa, R. E., Ruiz-Matuk, C., Bello-Figueroa, M. B., Polanco, K., Salado, D., Carrion, V., Pantaleon Vásquez, J., Vargas Bocio, P., Garcia, R., Sánchez Almánzar, E. (2025). Factores modificables y determinantes asociados un mal control lipídico en individuos con alto riesgo cardiovascular. Ciencia y Salud, 9(3), 51-67. https://doi.org/10.22206/cisa.2025.v9i3.3228
Resumen
Introducción: La ciencia continúa aportando evidencia en el manejo de la enfermedad cardiovascular en pacientes de alto riesgo. Este estudio tuvo como objetivo identificar factores modificables y determinantes sociales de salud asociados al mal control lipídico. Metodología: es un estudio observacional y retrospectivo que incluyó 338 historias clínicas de individuos con casos nuevos de infarto al miocardio. Resultados: La población fue X(DE)= 68,3 (10,9) años. De las historias clínicas evaluadas, el 48,4% tiene antecedentes de dislipidemia y el 50,3% de Síndrome Coronario Agudo. La probabilidad de sufrir un evento coronario fue del 57,3% en pacientes con HTA (OR=57,3, p<0,001) y con antecedentes de ACV y enfermedad renal crónica (OR=9,10, p=0,038). El 4,2% (n = 11) de los pacientes recibieron monoterapia con estatinas de baja intensidad y ninguno de ellos recibió terapia de alta intensidad combinada con ezetimiba. En el 20,4% (n = 69) de los pacientes se observó una reducción de la dosis del tratamiento y en el 2,1% (n = 7) de los casos se añadió una nueva medicación. Solo el 31,95% (n = 108), p < 0,01, alcanzó niveles de c-LDL inferiores a 70 mg/dl en el período de estudio. Cada punto de aumento en el nivel de colesterol LDL se asoció con un aumento aproximado del 6% en angina inestable/infartos de miocardio en comparación con las categorías de frecuencia más baja. Conclusión: Existe una necesidad apremiante de protocolizar y establecer planes de adherencia para reducir los niveles de c-LDL en personas con alto riesgo cardiovascular.
Palabras clave: Colesterol, estatinas, enfermedades cardiovasculares, infarto al miocardio.
Abstract
Introduction: Science continues to provide evidence in managing cardiovascular disease in high-risk patients. This study aimed to identify modifiable factors and social determinants of health associated with poor lipid control. Methodology: This observational and retrospective study included 338 medical records of individuals with new cases of myocardial infarction. Results: The population was X(SD)= 68.3 (10.9) years. Of the medical records evaluated, 48.4% had a history of dyslipidemia, and 50.3% had Acute Coronary Syndrome. The probability of suffering a coronary event was 57.3% in patients with hypertension (OR=57.3, p<0.001) and with a history of stroke and chronic kidney disease (OR=9.10, p=0.038). 4.2% (n = 11) of patients received low-intensity statin monotherapy, and none received high-intensity combined therapy with ezetimibe. Dosage reduction was observed in patients 20.4% (n = 69), and a new medication was added in 2.1% (n = 7). Only 31.95% (n = 108), p < 0.01, achieved LDL-C levels below 70 mg/dL during the study period. Each point increase in LDL-C level was associated with an approximate 6% increase in unstable angina/myocardial infarctions compared with the lowest frequency categories. Conclusion: There is an urgent need to protocolize and establish adherence plans to reduce LDL-C levels in individuals at high cardiovascular risk.
Keywords: Cholesterol, statin, cardiovascular diseases, myocardial infarctions.
Introduction
According to the World Health Organization (WHO), in 2019, the leading cause of death globally was heart disease, which was responsible for approximately 17.9 million deaths (1). Most deaths related to this issue occur in countries with lower and middle incomes (LMIC) (2). Cardiovascular disorders are the cause of 85% of deaths resulting from myocardial infarction (MI) and cerebrovascular accident (CVA), and one-third of all cardiovascular events occur in individuals below 70 years of age (2). These mortality rates from atherosclerotic cardiovascular disease (ASCVD) can be reduced by addressing modifiable risk factors, such as diet, exercise, and smoking, while also improving health systems to ensure effective monitoring of lipid levels, particularly in individuals with underlying comorbidities1.
In Latin America and the Caribbean (LAC), there has been an increase in the frequency of chronic illnesses among adults, and ASCVDs are responsible for most deaths2. Addressing behavioral risk factors can prevent ASCVDs, and the association between low-density lipoprotein cholesterol (LDL-C)3 and triglycerides (TGCs)4 plays a significant role in modifying ASCVD risk5 and atherogenic dyslipidemia6. A study conducted in the Dominican Republic (DR) highlighted alarming levels of dyslipidemia in the general population. The study found elevated LDL-C and triglyceride levels, reflecting the severity of the problem. It also revealed a 30.7% prevalence of low high-density lipoprotein cholesterol (HDL-C), significantly higher in men than in women, and a 21% prevalence of hypertriglyceridemia, which was also more common in men7.
Additionally, studies suggest that familial hypercholesterolemia (FH) contributes to cardiovascular events at a young age8, 9. Early detection, treatment, and lifestyle interventions are essential in these participants10, 11. With a high prevalence of 1 in 250 people, FH is considered one of the most common genetic diseases but remains underdiagnosed, especially in LMIC, where there is limited data regarding genetic population profiles11.
To reduce ASCVD morbidity and mortality, studies suggest that early LDL-C reduction and more intensive statin therapy following MI are associated with a lower risk of cardiovascular outcomes and all-cause mortality. Adherence to dyslipidemia management guidelines by healthcare professionals is also essential12. While the recommended LDL-C range is 1.4 mmol/L (55 mg/dL)13, 14, treatment adherence is challenging in developing countries due to various factors. These challenges are compounded by the high prevalence of cardiovascular risk factors, such as hypertension (HTN), diabetes mellitus (DM), and smoking, which are prevalent in Latin American countries and comparable to those seen in the United States for adjusted age15.
Given these challenges, this study aims to determine the prevalence of modifiable risk factors and lipid control and management in adults with increased cardiovascular risk in the Dominican Republic. It also seeks to explore decision-making processes and disparities in managing dyslipidemia in individuals at very high risk (VHR).
Methods
Study design
This study is a comprehensive, retrospective, hospital-based observational analysis of new acute myocardial infarction (AMI) cases in patients who underwent left heart coronary catheterization.
Settings
Data was collected from clinical records of cases between January 2017 and December 2021 at the coronary intervention unit of a third-level healthcare center located in Santo Domingo, the capital of the Dominican Republic. This center specializes in cardiometabolic conditions for adults and children and serves as a referral hospital for cases nationwide.
Participants
The estimated sample size was 309 cases, assuming a precision of 5% and a confidence level of 95%. We included 338 participants because we expected a 10% attrition rate. The criteria for the retrieved data registry included age > 18 years and previous use of lipid-lowering therapy associated with or recommended for any cardiovascular condition, evaluating the clinical records of participants who had undergone left heart coronary catheterization in the last 4 years.
Variables
The study’s primary outcome was to assess the prevalence of modifiable risk factors and lipid control in adults with elevated cardiovascular risk. This information is a basis for further research and can guide healthcare professionals in managing cardiovascular risks.
To determine the risk of future ASCVD events of the patients according to the AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol [16], we collected data from electronic records regarding major ASCVD events, including Recent ACS within the past 12 months, history of myocardial infarction, history of ischemic stroke, symptomatic peripheral arterial disease (history of claudication with ABI <0.85, or previous revascularization or amputation). High-risk conditions that were taken into account include: age > 65 years old, heterozygous familial hypercholesterolemia, history of prior coronary artery bypass surgery or percutaneous coronary intervention outside of the major ASCVD events, diabetes mellitus, hypertension, chronic kidney disease, current smoking, persistent elevated LDL-C despite maximally tolerated statin therapy and ezetimibe, and history of congestive heart failure. Based on the guidelines, we classified patients with 2 or more major ASCVD events or 1 major ASCVD event and 2 or more high-risk conditions as very high-risk (VHR). In contrast, the patients who did not meet the criteria were included in the High-Risk group (HR).
Data sources
The participants were classified according to the American Guidelines on the Management of Blood Cholesterol14, which classifies individuals as high CVD risk (HR) and very high CVD risk (VHR). Cardiovascular risk was determined based on major atherosclerotic cardiovascular disease (ASCVD) events, recent acute coronary syndrome (ACS) within the past 12 months, a history of myocardial infarction (MI) unrelated to the current ACS event, and a history of ischemic.
Ethical considerations
Ethical approval was obtained from the following committees: Universidad Iberoamericana (CEI2022-14), Centro de Diagnóstico Medicina Avanzada y Telemedicina (CEDIMAT, CEI-599), and the National Council of Bioethics in Health (CONABIOS 036-2022). These committees operate according to the Belmont Report principles, prioritizing respect for persons, justice, and beneficence.
Statistical methods
Continuous variables were described using medians with interquartile ranges for skewed data. Nonparametric tests were used, and categorical variables were presented as frequencies. For demographic, clinical, and therapeutic management, as well as the LDL-C levels described, lipid-lowering treatment used the proportions or median of demographics, and multiple logistic and ordinal regression analyses of clinical characteristics and mortality factors were performed. A binomial logistic regression model was used to investigate whether the type of therapy and time between the first CVA and the subsequent visit predicted MI events in this population. All analyses were performed using the Jamovi and R Software. Statistical significance was set at p < 0.05. significant. All statistical tests were two-tailed.
Results
The mean (SD) age was 68.3 (10.9) years, and 67.2% of the population was male. The most frequent comorbidity was HTN (84.0%), followed by DM (42.0%), and 20.2% of the patients were current smokers (Table 1).
Table 1. Description of Study Cohort and Medications Stratified by Cardiovascular Risk
VARIABLE |
HR (n=73) |
VHR (n=265) |
p-value |
Effect size |
SEX |
||||
Male |
47 (64.4%) |
180 (67.9%) |
0.568 b |
OR=0.579 |
Female |
26 (35.6%) |
85 (32.1%) |
||
AGE (years) |
0.056 a |
D Cohen=0.210 |
||
Mean ± S.D |
66.5± 10.8 |
68.9 ±11.1 |
||
CIVIL STATUS |
||||
Single |
56 (76.7%) |
227 (85.7%) |
0.149 b |
OR=0.570 |
Married |
16 (21.9%) |
37 (14%) |
||
Unknown |
1 (1.4%) |
1 (0.38%) |
||
SMOKING |
||||
Current smoker |
7 (9.6%) |
28 (10.6%) |
0.808 b |
C= 0.036 |
Former smoker |
13 (17.8%) |
55 (20.8%) |
||
Non Smoker |
53 (72.6%) |
182 (68.7%) |
||
ALCOHOL CONSUMPTION |
||||
Yes |
24 (32.9%) |
72 (27.2%) |
0.338 b |
C=0.052 |
No |
49 (67.1%) |
193 (72.8%) |
||
COMORBIDITIES |
||||
HTN |
51 (15.1%) |
233 (68.9%) |
<0.001 b |
OR=1.34 |
DM |
28 (38.3%) |
114 (43%) |
0.475 b |
OR=0.193 |
CKD |
3 (4.1%) |
17 (6.4%) |
0.460 b |
OR=1.60 |
Past history of dyslipidemia |
15 (20.5%) |
74 (27.9%) |
0.205 b |
OR=1.50 |
Past history of ACS |
35 (10.4%) |
135 (39.9%) |
0.650 b |
OR=1.13 |
Past history of CVA |
0 |
15 (5.7%) |
0.038 b |
0R=9.10 |
MEDICATION |
||||
Moderate-intensity statin monotherapy |
8 (10.9%) |
53 (20%) |
0.023a |
C=0.148 |
High-intensity statin monotherapy |
65 (89.1%) |
201 (75.8%) |
||
High-intensity statin + Ezetimibe combination therapy |
0 (0.0%) |
10 (3.8%) |
||
CHANGES IN TREATMENT |
||||
Substitution of drug |
4 (5.5%) |
24 (9.1%) |
0.397a |
C=0.135 |
Increase in dose |
4 (5.5%) |
34 (12.8%) |
||
Addition of a new drug |
1 (1.4%) |
6 (2.3%) |
||
Decrease in dose |
19 (26%) |
50 (18.9%) |
||
Removing of a drug |
2 (2.7%) |
9 (3.4%) |
||
No changes |
43 (58.9%) |
142 (53.6%) |
||
Notes: Kidney Disease; ACS: Acute Coronary Syndrome; CVA: cerebral vascular accident.
a T Student Test.
b Chi Square Test; OR: Odds Ratio; C: contingency coefficient.
The results of this investigation identified a critical gap in the management of dyslipidemia in participants at high cardiovascular risk. Despite the use of statins during follow-up, only 31.95% of participants achieved adequate LDL-C levels below 1.8 mmol/L (70 mg/dL), and only 12.9% achieved optimal levels <1.4 mmol/L (55 mg/dL), as recommended by clinical management guidelines (figure 1). This suboptimal control was highly associated with the recurrence rate of acute coronary syndromes, especially in individuals with a family history of cardiovascular disease (table 2). These findings, however, provide a promising direction for future dyslipidemia management.
Figure 1. LDL-c target achievement according to the ASCVD risk and type of therapy of the patient
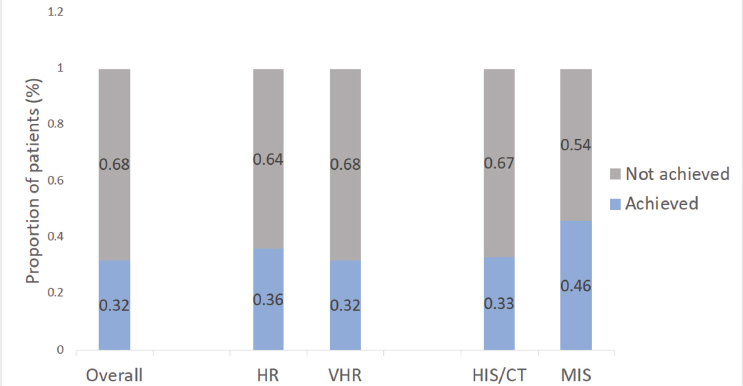
Notes: HR: High risk, VHR: Very high risk, HIS: High intensity statin therapy, CT: Combined therapy, MIS (Moderate intensity therapy). ASCVD: Atherosclerotic Cardiovascular Disease
Table 2. Outcomes in Acute Coronary Syndrome with HCVR and Use of Statins According to Therapeutic Intensity
Pharmacotherapy |
Outcomes (n=309) |
X2 |
p-value |
Contingency coefficient |
|
ACS recurrence* |
|||||
Yes n (%) |
No n (%) |
||||
High intensity statin |
137 (44.3) |
129 (41.7) |
3.03 |
0.220 |
0.095 |
Moderate intensity Statin |
24 (7.8) |
26 (8.4) |
|||
Combined therapy** |
6 (1.9) |
4 (1.3) |
|||
LDL-c goal< 70mg/dL |
|||||
Not achieved |
Achieved |
||||
High intensity statin/Combined therapy |
166 (53.7) |
86 (27.8) |
7.41 |
0.025 |
0.153 |
Moderate intensity Statin |
26 (8.4) |
22 (7.1) |
|||
Combined therapy** |
9 (2.9) |
0 |
|||
Survival status |
|||||
Deceased |
Alive |
||||
High intensity statin/Combined therapy |
4 (1.3) |
262 (84.8) |
3.15 |
0.207 |
0.096 |
Moderate intensity Statin |
3 (0.9) |
57 (18.4) |
|||
Combined therapy** |
0 |
10 (3.2) |
|||
Note:
* ACS: Acute Coronary Syndrome.
** Statin and fibrates
Of all participants at HR and VHR, only 33% reduced their LDL-C levels using high-intensity statins and combination therapy (Figure 1) and 46% using moderate-intensity statins. Thus, the study population had already been treated with statins. Notably, statin dose reductions were performed in 20.4% of cases during the study period without the specific reasons in the clinical record. In addition, 94.9% (n=321, p< 0.01) of participants received pharmacological treatment during the study period.
In the files evaluated, 2.07% (n=7) of deaths were related to coronary events (p<0.01). The ACS recurrence rate per 1000 persons/year for individuals at high ASCVD risk was lower than for individuals at HR (120 and 130, respectively) (Figure 2A). The rate of every 1000 persons/year of new events and deaths from all causes was higher in individuals with the highest CV risk, with a total of six (Figures 2A and B).
Figure 2. The recurrence of ACS in patients is classified according to their ASCVD risk level (A), and the incidence rate of a new ACS event and all-cause death in patients is classified according to their ASCVD risk level (B)
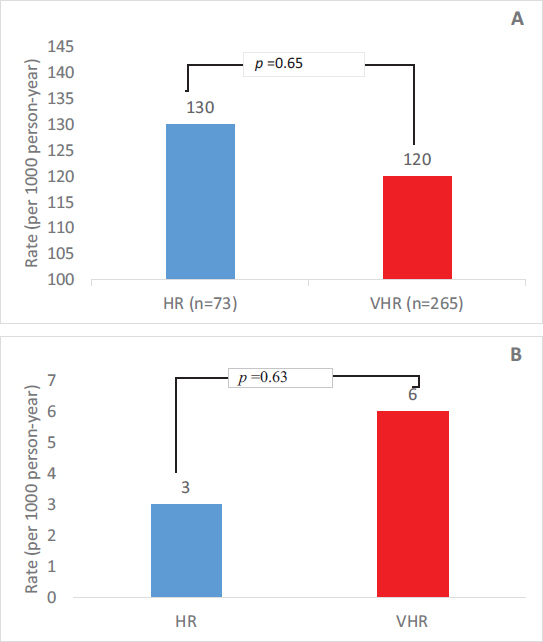
Notes: ACS: Acute coronary syndrome; ASCVD: Atherosclerotic Cardiovascular Disease; HR: High risk; VHR: Very high risk.
According to the American guidelines criteria, participants classified as HR were 21.6% and VHR 78.4%, respectively. The risk of cardiovascular disease was assessed by considering major ASCVD events and recent ACS that occurred in the last 12 months16, history of AMI other than current ACS events, and history of ischemic CVA. Participants who were considered HR had a history of either coronary artery bypass surgery or percutaneous coronary intervention and were over 65 years of age. The observation of interventions was performed without any relevant ASCVD events, DM, HTN, or current tobacco use (Table 1).
Participants with VHR of CVD on low-intensity statin monotherapy comprised 4.2% (n=11), and none of the individuals evaluated as HR were on high-intensity therapy combined with ezetimibe. In all the assessed clinical registries, a reduction in the treatment dose was evident in 20.4% (n=69) of the participants, with the addition of a new medication in 2.1% (n=7); 6.51% (n=22, p <0.001) had a CVA, and 94.9% (n=321, p <0.001) received lipid-lowering treatment for the first event of the AMI.
Moreover, only 31.95% (n=108, p < 0.01) reached LDL cholesterol levels less than 1.8 mmol/L (70 mg/dL). The median LDL-C level was 2.2 mmol/L (85.6 mg/dL). Evaluating all participants during follow-up consultations, 87.87% (n=297) presented with CVA (p<0.001), and 50.3% (n=170) had a coronary event (p=0.957). A secondary analysis excluded incomplete data related to more than one follow-up visit to evaluate the recurrence of cardiovascular events from the total (n=338) medical records, leaving 309 complete records (Table 2).
Of the individuals evaluated in the complete follow-up visits (n=309), 44.9% with the high cardiovascular risk presented a recurrence of ACS (Table 2), even when using high-intensity statins. In combination therapy with high-intensity statins and other lipid-lowering treatments, 56.6% of high-risk patients did not reach levels <1.8 mmol/L (<70 mg/dL). However, 75.8% was high-intensity statin monotherapy. The proportions of participants taking different statins were 70.6% atorvastatin, 19.6% rosuvastatin, 7.7% simvastatin, and 1.5% other combinations (see supplemental data). According to the clinical records, 80.9% of participants survived their first cardiovascular event (Table 2). Of the records evaluated, only 12.9% reached LDL-C levels <1.4 mmol/L (<55 mg/dL).
In individuals with a family history of ASCVD, 32% reached LDL levels of 1.8 mmol/L (<70 mg/dL), with an ACS recurrence of 57% and a mortality of 4% (Table 3).
Table 3. Outcomes Distribution in Patients with ASCVD Family History
Outcome |
ASCVD Family History |
p-value |
|
Positive (n=136) |
Negative (n=167) |
||
LDL-c goal (<70 mg/dL) |
|||
Achieved |
44 (32%) |
53 (32%) |
0.66 |
Not achieved |
78 (57%) |
105 (63%) |
|
ACS* recurrence |
|||
Yes |
78 (57%) |
74 (44%) |
0.024 |
No |
58 (43%) |
93 (56%) |
|
Discharge status |
|||
Deceased |
4 (3%) |
2 (1%) |
0.279 |
Alive |
132 (97%) |
165 (99%) |
|
Note: * ACS: Acute Coronary Syndrome
Although the individuals did not reach the standard levels required by the management guidelines, only 5.3% (n=18) and 5.6% (n=19) developed a second or third event, respectively. Among the total sample with coronary events, 78.4% (n=265) had a single event. Logistic regression was performed that did not show a significant relationship between the predictors related to the number of coronary events and variables such as heart rate (p=0.522), blood glucose level (p=0.266), and systolic blood pressure (p=0.203).
We conducted this study to determine whether LDL-C, triglyceride, and HDL-C levels could predict the likelihood of unstable angina/MI in patients with low adherence to lipid-lowering treatment and reduced follow-up visits. To this end, we used an ordered logit model. The predictors explained significant variance in the outcome (likelihood ratio χ2= 31.38, p = 0.041). Only the LDL cholesterol level (B = 0.006, SE = 0.002, OR = 1.007, p= 0.026) significantly and independently predicted the number of unstable angina/myocardial infarctions. Each point increase in the level of LDL-C registered was associated with a 6% increase in unstable angina/MI compared to the lower frequency categories. Overall, the model accounted for approximately 1% of the outcome variance (McFadden’s pseudo-R2 = 0.0102).
A binomial logistic regression model was used to investigate whether the type of therapy and time between the first CVA and the subsequent visit predicted MI events in this population. The data predictors were able to explain a significant portion of the variation in the outcome (likelihood ratio χ2(6) = 21.6, p < 0.001). The time between the first CVA and the subsequent visit significantly independently predicted MI events (B = 0.578, SE = 0.177, OR = 1.783, p= 0.001). Although not significantly related to the types of lipid-lowering therapy, it was found that PCSK9 inhibitors, compared to statins, could be a good predictor of MI events (OR = 7.166, B = 1.969, p= 0.149). Each point increase in time between the first CVA event registered was associated with about a 78% increase in the probability of an MI event. Overall, the model accounted for approximately 9% of the outcome variance (McFadden’s pseudo-R2 = 0.0939).
Discussion
Our findings contribute to the growing body of evidence on the management of dyslipidemia in low- and middle-income countries, demonstrating that even with high-intensity statin therapy, a significant proportion of patients fail to achieve recommended LDL-C targets17, 18. This highlights the urgent need for comprehensive strategies that address patient adherence, health system barriers, and timely initiation of therapy, as pharmacological treatment alone may be insufficient. Furthermore, the strong association between a family history of ACVD and increased recurrence of ACS events reinforces the need to integrate genetic risk assessment into routine clinical practice, particularly in regions where familial hypercholesterolemia remains underdiagnosed19.
It is crucial to note that data from multiple studies consistently demonstrate that individuals with LDL levels falling below the optimal range are not just high-risk but also very high-risk. This is a significant finding as it underscores the potential severity of the situation. Although beneficial, using lipid-lowering agents or therapeutic combinations for this purpose creates a gap when applying guide recommendations20–23.
Some evidence suggests that very high-risk participants have an increased risk of ACS recurrence and death compared to high-risk participants because of not reducing LDL-C levels to below 1.8 mmol/L (< 70 mg/dL)24, 25. However, there was a very similar incidence rate among both groups in the population studied, and even though VHR participants had a higher all-cause mortality rate than HR individuals, the minimum differences led to no significant p-value. These findings suggest poor health control beyond pharmacotherapy, leading to accelerated ASCVD status deterioration in both HR and VHR participants.
Our results support the association between a family history of ASCVD and patient health outcomes. The presence of a first-degree relative with previous ASCVD significantly correlated with patient’s recurrence of the disease (p<0.024). These findings align with those of earlier studies that consider a family history of early-onset ASCVD in first-degree relatives as an independent risk factor in survivors of AMI. Importantly, our research demonstrated that incorporating family history information can enhance the performance of a validated risk prediction model for recurrent ASCVD, emphasizing the necessity of considering this factor in clinical practice26.
In our data, a higher percentage of current smokers in the VHR category were reported rather than HR (10.6% vs. 9.6%, respectively). A more significant proportion of ex-smokers were in the VHR category than in the HR category (20.8% and 17.8%, respectively)27. A study reporting similar findings in current smokers pertained to the VHR group at 37% and the non-VHR at 27%28. A population-based study seeking to improve participants with ASCVD reported a significantly higher percentage of current smokers in the VHR group than in the non-VHR group (50% vs. 33%, respectively; p<0.001)24, 29.
This study demonstrated that HTN is more frequent in participants categorized as VHR (p<0.001). It is also known that having another CVA event, specifically ischemic stroke, and increased systolic blood pressure directly correlate with the ASCVD incident rate (p<0.001)30. The distribution of individuals with diabetes was analyzed among HR or VHR status (43% and 38.3%, respectively). Some studies focusing on the risk of ASCVD in participants with type 2 diabetes mellitus have concluded that there is a 20 to 23% higher risk of developing a first ASCVD event or a future ASCVD event31, 32.
There is evidence that adding an adjuvant drug to statin therapy as secondary prevention for high-risk individuals has a better outcome with an LDL-C target level of 1.8 mmol/L (< 70 mg/dL)21. The additional use of an inhibitor of PCSK9 or an interfering RNA molecule decreases LDL-C by an additional < 0.8 mmol/L (< 30 mg/dL) or 50% of baseline LDL-C levels33. It is also associated with reduced cardiovascular-related deaths34. Our research suggests that using PCSK9 inhibitors helps optimize a seven-fold reduction in cholesterol levels and the risk of cardiovascular outcomes, as in other studies35, 36. However, the participant records reported a low percentage of PCSK9 inhibitor use. This might be associated with medication costs, availability, adherence, and providers’ awareness of the medication benefits that reduce the risk of ASCVD.
Conclusions
Understanding the modifiable and non-modifiable factors associated with cardiovascular diseases (CVDs) is essential when analyzing programmatic interventions, especially in low- and middle-income countries (LMICs). Several factors contribute to the prevalence of CVD in these regions, and addressing them is crucial for improving outcomes. Physicians’ decision-making is a factor that must be addressed with the standardization of treatments, as well as a systematic review of the application of these guidelines. Disparities in access to the treatment of dyslipidemia are another face of the crisis in the primary care of these conditions. This may be a determining factor for the optimization of the prevention of cardiovascular diseases.
One notable finding of this study was that despite changes in serum LDL-C levels, no adjustments in therapy were made for either group, with this lack of modification remaining the most prevalent trend. The study also demonstrated a low mortality rate among the patient groups, particularly regarding the relationship between discharge status and pharmacotherapy. However, it is essential to emphasize that the final medical outcomes for individuals treated in the unit should be reported during follow-up consultations, which is an area that could benefit from enhanced reporting.
As noted in other studies34, 35, levels have been shown to predict coronary events, especially in patients undergoing elective percutaneous coronary intervention (PCI). Another significant predictor was the time between the coronary event and the first specialized visit, directly correlating with the number of future coronary events. This highlights the necessity of timely intervention and enhanced education to minimize care delays. The lack of information contributing to this delay represents a gap that future research should aim to address.
Although these individuals require constant cholesterol-lowering therapy, this study demonstrated nonadherence to management guidelines and interruption of treatment. The apparent cause of This could be attributed to three factors.
We propose evaluating these issues using a biosocial approach, including client-centered structural and behavioral interventions. This might be a good setting for a discussion that includes the following:
1.Awareness of international and national guidelines among healthcare providers, especially those specializing in cardiovascular care. This can be overcome by continuing medical education programs, health promotion, and follow-up of compliance with the guidelines of the Ministry of Health.
2.Although health insurance typically covers these medications, limitations prevent comprehensive coverage. To address this issue, we propose special programs that provide insurance coverage throughout the year for individuals with high-risk cardiovascular disease, potentially alleviating this barrier to adherence.
3.Among the modifiable interventions addressing behavioral changes, we must pave the way for a more comprehensive and integrated approach to medical care, which can be challenging when transporting patients from home to the health center and with associated costs. Other factors that limit care include waiting times for all medical care visits in patients with multiple comorbidities. We recommend creating more specialized care programs like home visits and telemedicine in peripheral centers. Another recommendation is to create a strategy for organizing specialized medical appointments in which multiple specialists can see the patient on the same day for high-risk individuals.
The genetic profile of a family history of ASCVD in the Dominican population is unknown as a non-modifiable factor. To our knowledge, Dominican files are scarce and do not necessarily focus on health issues. With their potential to revolutionize healthcare practices, this study’s findings could inform and significantly improve healthcare practices in tertiary healthcare centers specializing in this condition.
This research demonstrates the significant gap in the treatment of dyslipidemia in the high cardiovascular-risk population, highlighting the need to optimize decision-making and adherence to evidence-based management guidelines. It is also an invitation to identify disparities in treatment, ensuring permanent coverage of these therapeutic interventions and reducing cardiovascular events and mortality. On the clinical side, it is vital to strengthen the multidisciplinary approach and be more intentional in continuing medical education programs. Also, implementing modern therapeutic intervention programs, such as PCSK9 inhibitors, is necessary to integrate these molecules into health services. This study lays the groundwork for investigating the impact of social determinants on cardiovascular disease in a Latin context, being a tool to establish culturally adapted, optimized therapies.
Acknowledgments
We thank CEDIMAT and Dr. Julia Rodriguez for allowing us to conduct this research at their medical center and Dr. Robert Paulino for accompanying us during the manuscript.
Funding
This work was supported by NOVARTIS, Inc.
CRediT authorship contribution statement
Jenny Cepeda-Marte: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, writing original draft, Writing review & editing. Ricardo E. Hernández-Landa: Supervision, Validation, Visualization, writing original draft, Writing review & editing. Carlos Ruiz-Matuk: Data curation, Formal analysis, Writing original draft, Writing review & editing. Marc B. Bello-Figueroa: acquisition,Writing original draft, Writing review & editing. Kristy Polanco: acquisition,Writing original draft, Writing review & editing. Daniela Salado: Methodology, Project administration, Resources. Valery Carrion: Methodology, Project administration, Resources. Roberto Garcia; Conceptualization, Methodology. Pedro Vargas Bocio: Conceptualization. Elizabeth Sánchez Almánzar: Visualization. All authors reviewed the results and approved the final version of the manuscript.
Ethics
We obtained approval from the ethics committees of the Universidad Iberoamericana (CEI2022-14), Centro de Diagnóstico Medicina Avanzada y Telemedicina, CEDIMAT (CEI-599), and the National Council of Bioethics in Health (CONABIOS 036-2022). Ethics committees are governed by the Belmont and Helsinki Report principles, prioritizing respect for people, justice, and charity.
Disclaimer
The conclusions of this article are the sole responsibility of the authors and do not necessarily reflect the opinions, policies, or positions of Ciencia y Salud, its editors, or the Instituto Tecnolómgico de Santo Domingo (INTEC).
References
1. World Health Organization. World Health Organization. 2021 [cited 2023 Dec 4]. Cardiovascular diseases (CVDs). Available from: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1
2. OECD/World Bank. PANORAMA DE LA SALUD [Internet]. [cited 2024 Jun 16]. Available from: https://www.oecd.org/health/panorama-de-la-salud-latinoamerica-y-el-caribe-2020-740f9640-es.htm
3. Figorilli F, Mannarino MR, Bianconi V, Pirro M. Cholesterol-Lowering Therapy in Patients at Low-to-Moderate Cardiovascular Risk. High Blood Pressure & Cardiovascular Prevention [Internet]. 2022 [cited 2024 Jun 16];29:327–36. Available from: https://doi.org/10.1007/s40292-022-00529-2
4. Hans-Willi PDMB. Low Density Lipoprotein Cholesterol and Coronary Heart Disease – Lower is Better. European Cardiology Review [Internet]. 2005 [cited 2023 Jun 2];1(1):1. Available from: https://www.ecrjournal.com/articles/low-density-lipoprotein-cholesterol-and-coronary-heart-disease-lower-better
5. Bartlett J, Predazzi IM, Williams SM, Bush WS, Kim Y, Havas S, et al. Is isolated low high-density lipoprotein cholesterol a cardiovascular disease risk factor? Circ Cardiovasc Qual Outcomes [Internet]. 2016 May 1 [cited 2024 Jun 16];9(3):206–12. Available from: https://pubmed.ncbi.nlm.nih.gov/27166203/
6. Ignacio C. Dislipidemia Aterogénica en Latinoamérica. Sociedad Interamericana de Cardiologia [Internet]. [cited 2024 Jun 16]; Available from: https://www.scielo.org.mx/pdf/rmc/v28n2/0188-2198-rmc-28-02-00057.pdf
7. Los Factores De Riesgo Cardiovascular Y Síndrome Metabólico E DE, Pichardo R, Principal I, González M ÁR, Ejecutivo C, Ramirez W, et al. Estudio Efricard II EFRICARD II [Internet]. 2011 [cited 2023 May 27]. Available from: https://static.elsevier.es/cardio/static/premio_cardio/revista-dominicana-cardiologia.pdf
8. Chlebus K, Zdrojewski T, Gruchała M, Gałąska R, Pajkowski M, Kocejko MR, et al. Cardiovascular risk factor profiles in familial hypercholesterolemia patients with and without genetic mutation compared to a nationally representative sample of adults in a high-risk European country. Am Heart J [Internet]. 2019 Dec 1 [cited 2023 Jun 2];218:32–45. Available from: https://pubmed.ncbi.nlm.nih.gov/31706143/
9. McGowan MP, Hosseini Dehkordi SH, Moriarty PM, Duell PB. Diagnosis and treatment of heterozygous familial hypercholesterolemia. J Am Heart Assoc [Internet]. 2019 [cited 2024 Jun 16];8(24). Available from: https://www.ahajournals.org/doi/10.1161/JAHA.119.013225
10. Romero Viamonte K, Chamorro Oña CR, Pimienta Concepción I, Molina M. Diagnóstico de hipercolesterolemia familiar. Criterios holandeses de la Organización Mundial de la Salud Diagnosis of familial hypercholesterolemia. Dutch criteria of the World Health Organization. Núm [Internet]. [cited 2024 Jun 16];(5). Available from: https://revista.uniandes.edu.ec/ojs/index.php/EPISTEME/article/view/817
11. Stoll M, Dell ’oca N, Stoll DM, Dell’oca N. Genética de la hipercolesterolemia familiar. Revista Uruguaya de Cardiología [Internet]. 2019 Feb [cited 2024 Jun 16];34(3):239–59. Available from: http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-04202019000300239&lng=es&nrm=iso&tlng=es
12. Al-Rasadi K, Al-Waili K, Al-Sabti A, Al-Hinai A, Al-Hashmi K, Al-Zakwani I, et al. Criteria for Diagnosis of Familial Hypercholesterolemia: A Comprehensive Analysis of the Different Guidelines, Appraising their Suitability in the Omani Arab Population [Internet]. Vol. 29, Oman Medical Specialty Board Review Article Oman Medical Journal. 2014 [cited 2024 Jun 16]. Available from: https://pubmed.ncbi.nlm.nih.gov/24715932/
13. Schubert J, Lindahl B, Melhus H, Renlund H, Leosdottir M, Yari A, et al. Low-density lipoprotein cholesterol reduction and statin intensity in myocardial infarction patients and major adverse outcomes: a Swedish nationwide cohort study. Eur Heart J [Internet]. 2021 Jan 20 [cited 2024 Jun 16];42(3):243–52. Available from: https://pubmed.ncbi.nlm.nih.gov/33367526/
14. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J [Internet]. 2020 Jan 1;41(1):111–88. Available from: https://doi.org/10.1093/eurheartj/ehz455
15. Miranda JJ, Herrera VM, Chirinos JA, Gómez LF, Perel P, Pichardo R, et al. Major Cardiovascular Risk Factors in Latin America: A Comparison with the United States. The Latin American Consortium of Studies in Obesity (LASO). PLoS One [Internet]. 2013 Jan 17 [cited 2024 Jun 16];8(1). Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0054056
16. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation [Internet]. 2019 Jun 18 [cited 2023 Jul 11];139(25):E1082–143. Available from: https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000000625
17. Pavía-López AA, Alcocer-Gamba MA, Ruiz-Gastelum ED, Mayorga-Butrón JL, Mehta R, Díaz-Aragón FA, et al. Guía de práctica clínica mexicana para el diagnóstico y tratamiento de las dislipidemias y enfermedad cardiovascular aterosclerótica Mexican clinical practice guideline for the diagnosis and treatment of dyslipidemias and atherosclerotic cardiovascular disease. Arch Cardiol Mex [Internet]. 2022 [cited 2025 Feb 8];92:1–62. Available from: www.archivoscardiologia.com
18. Carbayo-Herencia EP, Carbayo-Herencia JA, Carbayo-Herencia EP, Carbayo-Herencia JA. Las actuales guías en el manejo de las dislipidemias europeas y estadounidenses no están de acuerdo en sus objetivos y recomendaciones. Journal of Negative and No Positive Results [Internet]. 2021 [cited 2025 Feb 8];6(7):898–925. Available from: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S2529-850X2021000700001&lng=es&nrm=iso&tlng=es
19. Krychtiuk KA, Ahrens I, Drexel H, Halvorsen S, Hassager C, Huber K, et al. Acute LDL-C reduction post ACS: strike early and strike strong: from evidence to clinical practice. A clinical consensus statement of the Association for Acute CardioVascular Care (ACVC), in collaboration with the European Association of Preventive Cardiology (EAPC) and the European Society of Cardiology Working Group on Cardiovascular Pharmacotherapy. Eur Heart J Acute Cardiovasc Care [Internet]. 2022 Dec 1 [cited 2025 Feb 8];11(12):939–49. Available from: https://pubmed.ncbi.nlm.nih.gov/36574353/
20. Ray KK, Haq I, Bilitou A, Manu MC, Burden A, Aguiar C, et al. Treatment gaps in the implementation of LDL cholesterol control among high- and very high-risk patients in Europe between 2020 and 2021: the multinational observational SANTORINI study. The Lancet Regional Health - Europe. 2023 Jun 1;29.
21. Vrablík M, Šarkanová I, Breciková K, Šedová P, Šatný M, Tichopád A. Low LDL-C goal attainment in patients at very high cardiovascular risk due to lacking observance of the guidelines on dyslipidaemias. PLoS One [Internet]. 2023 [cited 2023 Jun 1];18(5):e0272883. Available from: /pmc/articles/PMC10202298/
22. Blom DJ, Ranjith N, Joshi P, Joshi S, Naidoo P, van Tonder A, et al. The therapeutic management of South African dyslipidaemic patients at very high cardiovascular risk (CARDIO TRACK): a cross-sectional study. Cardiovasc J Afr [Internet]. 2020 Sep 1 [cited 2023 Jun 1];31(5):245. Available from: /pmc/articles/PMC8762769/
23. Kotseva K, Investigators on behalf of the E. The EUROASPIRE surveys: lessons learned in cardiovascular disease prevention. Cardiovasc Diagn Ther [Internet]. 2017 Dec 1 [cited 2023 Jun 1];7(6):633. Available from: /pmc/articles/PMC5752826/
24. Navar AM, Matskeplishvili ST, Urina-Triana M, Arafah M, Chen JW, Sukonthasarn A, et al. Prospective evaluation of lipid management following acute coronary syndrome in non-Western countries. Clin Cardiol [Internet]. 2021 Jul 1 [cited 2024 Jun 16];44(7):955–62. Available from: https://onlinelibrary.wiley.com/doi/10.1002/clc.23623
25. Fonarow GC, Kosiborod MN, Rane PB, Nunna S, Villa G, Habib M, et al. Patient characteristics and acute cardiovascular event rates among patients with very high-risk and non-very high-risk atherosclerotic cardiovascular disease. Clin Cardiol [Internet]. 2021 Oct 1 [cited 2023 Jun 1];44(10):1457–66. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/clc.23706
26. Kong NW, Bavishi A, Amaral AP, Tibrewala A, Jivan A, Silberman P, et al. Risk Differences in Secondary Prevention Patients Who Present With Acute Coronary Syndrome and Implications of Guideline-Directed Cholesterol Management. American Journal of Cardiology [Internet]. 2020 Oct 15 [cited 2024 Jun 16];133:1–6. Available from: https://pubmed.ncbi.nlm.nih.gov/32807385/
27. Wahrenberg A, Kuja-Halkola R, Magnusson PKE, Häbel H, Warnqvist A, Hambraeus K, et al. Cardiovascular Family History Increases the Risk of Disease Recurrence After a First Myocardial Infarction. Journal of the American Heart Association J Am Heart Assoc [Internet]. 2021 [cited 2023 Jun 6];10:22264. Available from: https://www.ahajo
28. Karmali KN, Ning H, Goff DC, Lloyd-Jones DM. Identifying individuals at risk for cardiovascular events across the spectrum of blood pressure levels. J Am Heart Assoc [Internet]. 2015 Sep 1 [cited 2023 Jun 1];4(9). Available from: https://www.ahajournals.org/doi/abs/10.1161/JAHA.115.002126
29. Zhao Y, Xiang P, Coll B, López JAG, Wong ND. Diabetes associated residual atherosclerotic cardiovascular risk in statin-treated patients with prior atherosclerotic cardiovascular disease. J Diabetes Complications [Internet]. 2021 Mar 1 [cited 2023 Jun 1];35(3):107767. Available from: /pmc/articles/PMC7870509/
30. Poudel B, Rosenson RS, Bittner V, Gutiérrez OM, Anderson AH, Woodward M, et al. Atherosclerotic Cardiovascular Disease Events in Adults With CKD Taking a Moderate- or High-Intensity Statin: The Chronic Renal Insufficiency Cohort (CRIC) Study. Kidney Med [Internet]. 2021 Sep 1 [cited 2023 Jun 1];3(5):722-731.e1. Available from: https://pubmed.ncbi.nlm.nih.gov/34693254/
31. Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. New England Journal of Medicine [Internet]. 2017 May 4 [cited 2024 Jun 16];376(18):1713–22. Available from: https://www.nejm.org/doi/full/10.1056/NEJMoa1615664
32. Ray KK, Landmesser U, Leiter LA, Kallend D, Dufour R, Karakas M, et al. Inclisiran in Patients at High Cardiovascular Risk with Elevated LDL Cholesterol. New England Journal of Medicine [Internet]. 2017 Apr 13 [cited 2024 Jun 16];376(15):1430–40. Available from: https://www.nejm.org/doi/full/10.1056/NEJMoa1615758
33. Khan SU, Yedlapati SH, Lone AN, Hao Q, Guyatt G, Delvaux N, et al. PCSK9 inhibitors and ezetimibe with or without statin therapy for cardiovascular risk reduction: a systematic review and network meta-analysis. BMJ [Internet]. 2022 May 4 [cited 2023 Jul 11];377. Available from: https://www.bmj.com/content/377/bmj-2021-069116
34. Hao Q, Aertgeerts B, Guyatt G, Bekkering GE, Vandvik PO, Khan SU, et al. RAPID RECOMMENDATIONS PCSK9 inhibitors and ezetimibe for the reduction of cardiovascular events: a clinical practice guideline with risk-stratified recommendations. [cited 2023 Jul 11]; Available from: http://dx.doi.org/10.1136/bmj-2021-069066
35. Chen X, Rong C, Qi P, Bai W, Yao W, Zhang Y, et al. LDL-C and Total Stent Length are Independent Predictors of Periprocedural Myocardial Injury and Infarction for Unstable Angina Patients Undergoing Elective Percutaneous Coronary Intervention. Int J Gen Med [Internet]. 2021 [cited 2023 Jul 11];14:1357. Available from: /pmc/articles/PMC8057801/
36. Zhong Z, Liu J, Zhang Q, Zhong W, Li B, Li C, et al. Relationship Between Preoperative Low-Density Lipoprotein Cholesterol and Periprocedural Myocardial Injury in Patients Following Elective Percutaneous Coronary Intervention in Southern China. Med Sci Monit [Internet]. 2018 Jun 18 [cited 2023 Jul 11];24:4154. Available from: /pmc/articles/PMC6038720/
_______________________________
1 MD. NL. Universidad Iberoamericana, Francia Street, 208. Santo Domingo, República Dominicana. ORCID: https://orcid.org/my-orcid?orcid=0000-0002-5758-863X, email: j.cepeda@prof.unibe.edu.do (autor de correspondencia)
2 MD. Universidad Iberoamericana, Francia Street, 208. Santo Domingo, República Dominicana. ORCID: https://orcid.org/0009-0007-8238-7331, email: rhernandez16@est.unibe.edu.do
3 PhD. Universidad Iberoamericana, Francia Street, 208. Santo Domingo, República Dominicana. ORCID: https://orcid.org/0000-0003-2681-4953, email: c.ruiz4@unibe.edu.do
4 MD. Universidad Iberoamericana, Francia Street, 208. Santo Domingo, República Dominicana. ORCID: https://orcid.org/0000-0003-1011-1487, email: mbello1@est.unibe.edu.do
5 MD. Universidad Iberoamericana, Francia Street, 208. Santo Domingo, República Dominicana. ORCID: https://orcid.org/0009-0001-1785-4032, email: kpolanco3@est.unibe.edu.do
6 BS. Universidad Iberoamericana, Francia Street, 208. Santo Domingo, República Dominicana. ORCID: https://orcid.org/0000-0001-5793-5518, email: dsalado@est.unibe.edu.do
7 MD. Universidad Iberoamericana, Francia Street, 208. Santo Domingo, República Dominicana. ORCID: https://orcid.org/0009-0003-6654-9514, email: carrionvalery32@gmail.com
8 MD. Universidad Iberoamericana, Francia Street, 208. Santo Domingo, República Dominicana. ORCID: https://orcid.org/0009-0002-7084-3444, email: Jpantaleon1@est.unibe.edu.do
9 MD. CEDIMAT Centro de Diagnóstico Medicina Avanzada y Telemedicina. Arturo Logroño, Plaza de la Salud. República Dominicana. ORCID: https://orcid.org/0000-0002-2114-6856, email: dr.pvargasb@gmail.com
10 MD. NOVARTIS Pharma CANDEAN, Guatemala City, Guatemala. ORCID: https://orcid.org/0009-0002-6749-663X, email: roberto.garcia@novartis.com
11 BS. Universidad Iberoamericana, Francia Street, 208. Santo Domingo, República Dominicana. ORCID: https://orcid.org/0009-0009-6325-4474, email: esanchez23@est.unibe.edu.do
