Introduction
Caroli’s disease is a rare condition, with a prevalence of 1 in 1,000,000 individuals1. It consists of a congenital affectation of the intrahepatic bile ducts, characterized by a multifocal and segmented dilatation2. The most common symptoms presented in the disease are right quadrant abdominal pain, jaundice, and cholangitis3. Diagnosis is established from imaging tests such as ultrasound, computed tomography (CT), and magnetic resonance cholangiopancreatography (MRCP)4. On the other hand, treatment for this disease remains controversial. It may consist of Roux-en-Y hepaticojejunostomy, liver resection, or liver transplant, depending on the characteristics of each patient5. However, currently the most recommended is to perform a partial hepatectomy or liver transplant2.
In the same way, the treatment with laparoscopic Roux-en-Y hepaticojejunostomy represents a promising and less invasive treatment technique for this disease. In this case report, the Hepp Couinaud video laparoscopic technique was used to provide conservative management and preserve the integrity of the patient’s liver.
Case
A 60-year-old woman visited the surgery department at our hospital due to onset of jaundice and diffuse abdominal pain. In the physical evaluation, she presented a temperature of 35 °C, a heart rate of 101 bpm, a blood pressure of 114/91 mmHg, and an oxygen saturation of 99%. In addition, mild jaundice, a depressible abdomen, and no pain on superficial or deep palpation were observed. She has a history of schizophrenia which is treated with clozapine (100 mg/day). She reported no family history or relevant surgical history. Laboratory tests showed Hemoglobin levels of 12.0 g/dL; hematocrit 34.8%; MCV 85 fL; HCM 29.6 pg; Neutrophils 61.6%, Lymphocytes 26.9%; Creatinine 0.47mg/dl; Urea 10 mg/dl; Amylase at 45 U/L; Lipase 25U/L; Alkaline Phosphatase (FFA) 306 U/L; Gamma Glutamyl Transferase (GGT) 894 U/L; TGO transaminase (AST) 14 U/L; TGP transaminase (ALT) 23 U/L.
Total abdominal ultrasonography reported liver of standard dimensions and contours, with homogeneous echotexture. The gallbladder was slightly distended, with thin walls and the presence of multiple stones inside. It showed evidence of a large dilatation of intrahepatic bile ducts with reverberation artifacts inside. The dilatation of the common bile duct, had a maximum caliber of 1.2 cm, without identifying any obstructive factor. Therefore, leaving a diagnostic impression of cholelithiasis with great dilation of intra and extrahepatic bile ducts without identified obstructive factors.
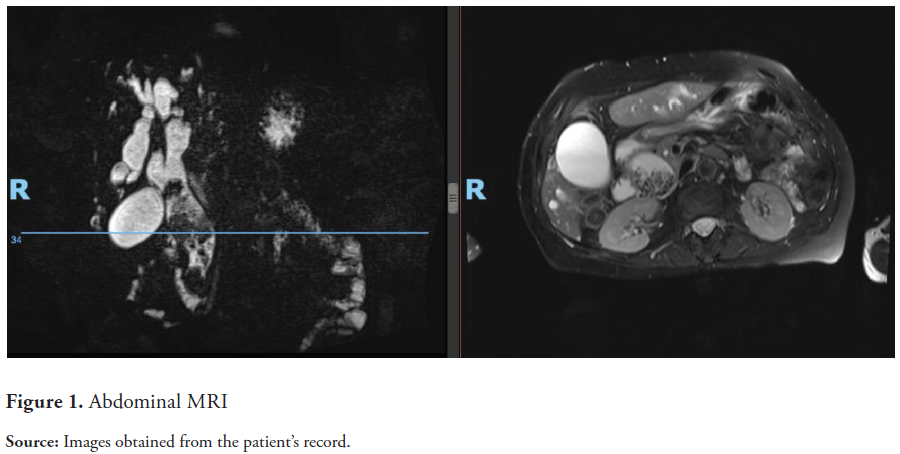
Due to the suspicion of Caroli’s disease, it was decided to perform MRCP to make an effective differential diagnosis and avoid confusion with similar pathologies such as primary sclerosing cholangitis, isolated polycystic liver disease, and hepatic cystic hamartoma. It was performed with a highly T2-weighted technique to assess the bile duct after intravenous gadolinium injection. In addition, axial images were obtained, evaluating T1, and T2, focusing on diffusion and coronal T2-weighted. It showed a partially distended, thin-walled gallbladder containing biliary sludge and several small stones (Figure 1). In addition, it showed a diffuse dilation of the intrahepatic and extrahepatic bile ducts with several microcalculi inside, with a predominance in the pathways of segments IVB and V. It presented an increased caliber up to 2.4 cm in diameter. Also, with micro stones up to 1.5 cm. The patient was diagnosed with Caroli’s disease.
With these findings, it was concluded that the patient had indications for surgical treatment. Although the gold standard treatment for this type of autoimmune disease is liver transplantation, it was not considered the best option due to cholestatic syndrome associated with cholangitis. Thus, it was decided to perform a Hepp Couinaud biliodigestive bypass by video laparoscopy with Roux-en-Y reconstruction.
The standard laparoscopic equipment used to perform this procedure included a 10mm 30° telescope to perform a choledochotomy and evaluate the bile ducts. In addition, the conventional fully laparoscopic multiport approach was adopted. The patient was placed in a supine position with the legs spread in the French position, and the surgeon positioned himself in the middle of the patient. Under general anesthesia, five 5 to 10-mm incisions were made.
An intraoperative examination confirmed the diagnosis of Caroli’s disease. The increased caliber of the common bile duct made it possible to identify the right and left hepatic ducts (Figure 2). An intraoperative frozen biopsy of the proximal border of the common bile duct was performed to exclude suspicion of malignancy. From this, the intra-choledochal and hepatic stones were removed with an exhaustive lavage with physiological solution and created a new hepato-biliary drainage route. When identifying the angle of Treitz, the small intestine was sectioned 50 cm upstream, thus creating the biliopancreatic, choledochojejunal upstream. The alimentary lift (latero-lateral entero-anastomosis) was subsequently performed with PDS 3-0. Operative time was 3 hours with minimal bleeding and no complications. Peri-anastomosis laminar tube drainage was placed.
The patient was periodically evaluated in the general surgery consultation every month. As a result, she did not present abdominal pain or any other complication in a follow-up period of 6 months after the surgical intervention.
Discussion
The diagnosis of Caroli’s disease is based mainly on imaging findings, in which distal dilatations of the intrahepatic bile ducts can be evidenced7. In this patient’s case, dilatation of the common bile duct and the intra and extrahepatic bile ducts was evident.
On the other hand, the treatment of choice for this disease is surgery such as segmentectomy, lobectomy, or hepaticojejunostomy7. Although previous studies report hepatic resection as an optimal treatment for most of those affected by Caroli’s disease8, it can have important consequences on the patient’s health. Among the most important repercussions is intraperitoneal hemorrhage, which affects up to 10% of patients undergoing hepatectomy. Another complication is bile leakage, which affects approximately 17%. Finally, the most feared consequence after resectioning a part of the liver is liver failure, which occurs in up to 33.83% of cases9.
In this case, a Hepp-Couinaud biliodigestive bypass was performed by video laparoscopy with Roux-en-Y reconstruction. This alternative significantly reduces the risk of bleeding and bile leakage10. In this patient, it was also considered because previous imaging studies showed bilateral dilatation of both the right and left intrahepatic ducts, with no evidence of liver fibrosis. The presence of an impacted stone in the distal common bile duct and the impossibility of removing it endoscopically (ERCP) was another point to be analyzed for our minimally invasive approach.
Conclusion
Caroli’s disease is an infrequent pathology with varying clinical complexity due to the extent of the disease, the location of pathological bile ducts, and the presence of complications. Radical surgery is the treatment of choice for localized diseases. However, the VLP biliodigestive bypass in patients with associated cholestatic syndromes should be considered a treatment prior to a more aggressive approach. The minimally invasive approach to Caroli’s disease requires extensive experience in liver surgery and complex biliary procedures. There is still little data in the literature on long-term results, so more studies are needed to confirm its effectiveness.

