Ciencia y Salud, Vol. VII, No. 2, abril-junio, 2023 • ISSN (impreso): 2613-8816 • ISSN (en línea): 2613-8824 • Sitio web: https://revistas.intec.edu.do/
IMPACT OF HORMONAL CONTRACEPTION ON FEMALE SEXUAL FUNCTION AMONG UNIVERSITY STUDENTS OF REPRODUCTIVE AGE IN THE DOMINICAN REPUBLIC: A CROSS-SECTIONAL STUDY
Impacto de la anticoncepción hormonal en la función sexual femenina entre estudiantes universitarias en edad reproductiva en República Dominicana: un estudio transversal
Cómo citar: . Verdeja-Vicente S, Villalona-Lluveres AR, Cepeda-Marte JL. Impact of hormonal contraception on female sexual function among university students of reproductive age in the Dominican Republic: A cross-sectional study. cysa [Internet]. 2023 Jun. 3 [cited 2023 Jun. 2];7(2):7-16. Available from: https://revistas.intec.edu.do/index.php/cisa/article/view/2842
1. Introduction
Hormonal contraceptives (HC) are the most popular method of contraception due to their high efficacy rate1. In 2019, the United Nations (UN) estimated that 248 million people worldwide use pill, injectable, and implant forms of hormonal contraception2. However, changes in sexual health, as well as androgenic insufficiency among HC users, have been reported3-6. Unlike other side effects of HC, its impact on users’ sexual function has not yet been studied as extensively. A better understanding of the relationship between HC use and sexual function is important as the decrease in sexual function is a reported cause of HC discontinuation by users4, 7. In the interest of providing women with greater understanding, safety, and control over their reproductive preferences, clinicians must be aware of the impact of these sexual side effects on adherence to the method when giving contraceptive counsel to their patients.
The association between the use of HC and the decrease in sexual function has been attributed to the elevation in the resulting levels of sex hormone-binding globulin (SHBG). Previous studies have discovered an increase in SHBG when using HC and a subsequent decrease in plasma androgens associated with female sexual function (FSF)7, 8. A study conducted in Sweden by Malmborg et al. (2016)4 found that the use of HC was linked to lower levels of female sexual function, and their users were more likely to discontinue them. Another European study conducted on medical students from various countries found lower levels of FSF in users of oral HC compared to other methods (including other hormonal methods)5, 6.
The Dominican Republic (DR) has one of the highest rates of undesired pregnancy in Latin America and the Caribbean9, yet, to the authors’ knowledge, the sexual side effects of HC have not yet been widely studied in this population. For this reason, the present study aims to determine whether HC has a negative impact on female sexual function (FSF) among university students, as well as identify the primary reasons for HC abandonment and levels of satisfaction from users.
1.1 Evaluation of Female Sexual Function
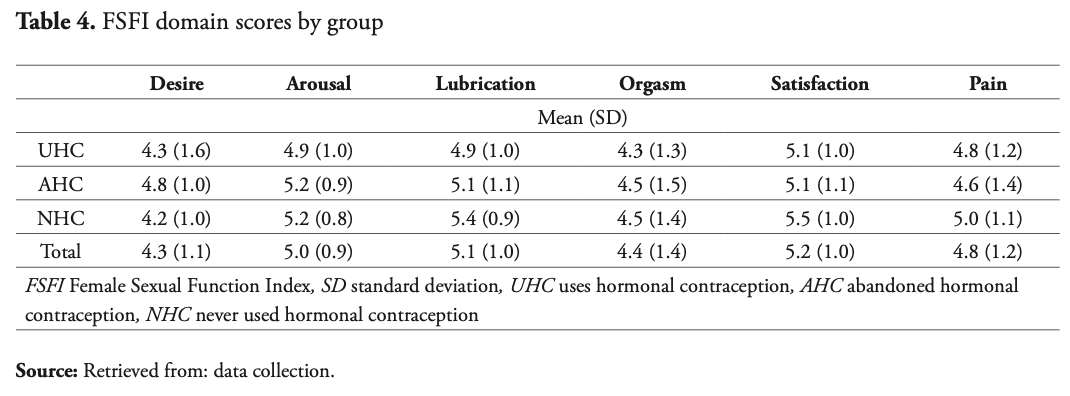
FSF is evaluated in six aspects: desire, arousal, lubrication, satisfaction, orgasm, and pain. In the scientific community, FSF has been studied using the Female Sexual Function Index (FSFI)5, 8, a validated score-based questionnaire that helps determine the risk of female sexual dysfunction (FSD).
2. Material and Methods
2.1 Study design, study population and ethics
A cross-sectional study was conducted, using a descriptive, questionnaire-based design. The study used snowball sampling to recruit a sample of 18- to 30-year-old female students enrolled at the Universidad Iberoamericana (UNIBE), a private institution of higher education located in Santo Domingo, Dominican Republic. A total sample of 251 participants was collected, meeting the following criteria: (1) being sexually active and (2) using a hormonal contraceptive method (CM) exclusively for contraception purposes. The exclusion criteria were the following: current pregnancy, use of psychoactive/anticonvulsive medication, chronic disease, current gynecological condition, and use of HC for non-contraceptive purposes. Participants were divided into three groups based on their relationship with HC: one comparison group made up of 80 participants (31.9%) who had never used HC (NHC), one study group composed of 132 (52.6%) current users of HC (UHC), and one study group composed of 39 (15.5%) participants who had abandoned HC (AHC). A 5.9% error margin and 95% confidence level were chosen.
The study took place after prior authorization from the Universidad Iberoamericana’s ethics committee (CEI2020-225), and consent was given by all participants through an online questionnaire. Study participation was advertised through medical student interest groups via a standardized email from the university’s institutional email service, including the study description and a questionnaire link. The anonymity of participants was maintained at all times. The questionnaire was distributed monthly and was made available for a period of seven months, from September 2020 to April 2021. No financial compensation or other incentives were given to the participants.
2.2 Online questionnaire
The study used an anonymous, self-administered online questionnaire for data collection which was designed using the CHERRIES internet survey checklist10. The questionnaire was divided into two parts. The first was composed of 21 general questions and 2-7 group-specific questions that were validated through a pilot test. The questionnaire included demographics, satisfaction with CM, fitness level, use of alcohol or tobacco, being in a steady relationship, sexual activity, and other general questions about their relationship with their CM. The second part incorporated 19 questions of the official Spanish version of the FSFI11, obtained and approved through ePROVIDE Mapi Research Trust, based on the sexual experience of participants during the last four weeks.
2.3 Data analysis
All data was processed using IBM SPSS Statistics 28 (Armonk, NY). Demographic and satisfaction data, as well as other data from the first part of the questionnaire, were summarized as either mean and standard deviation (SD), or number and percentage. The FSFI scores were calculated and reported as means for the domain and total scores. The Kruskal-Wallis test was used to determine the difference between the total FSFI scores of the study groups, while Mann-Whitney U was used to determine the difference in the scores of NHC and AHC groups. Spearman’s correlation was used to evaluate the difference between the percentages of participants at risk of sexual dysfunction, indicated by a FSFI total score <26.5512.
3. Results
3.1 Study population, demographics and types of contraceptives
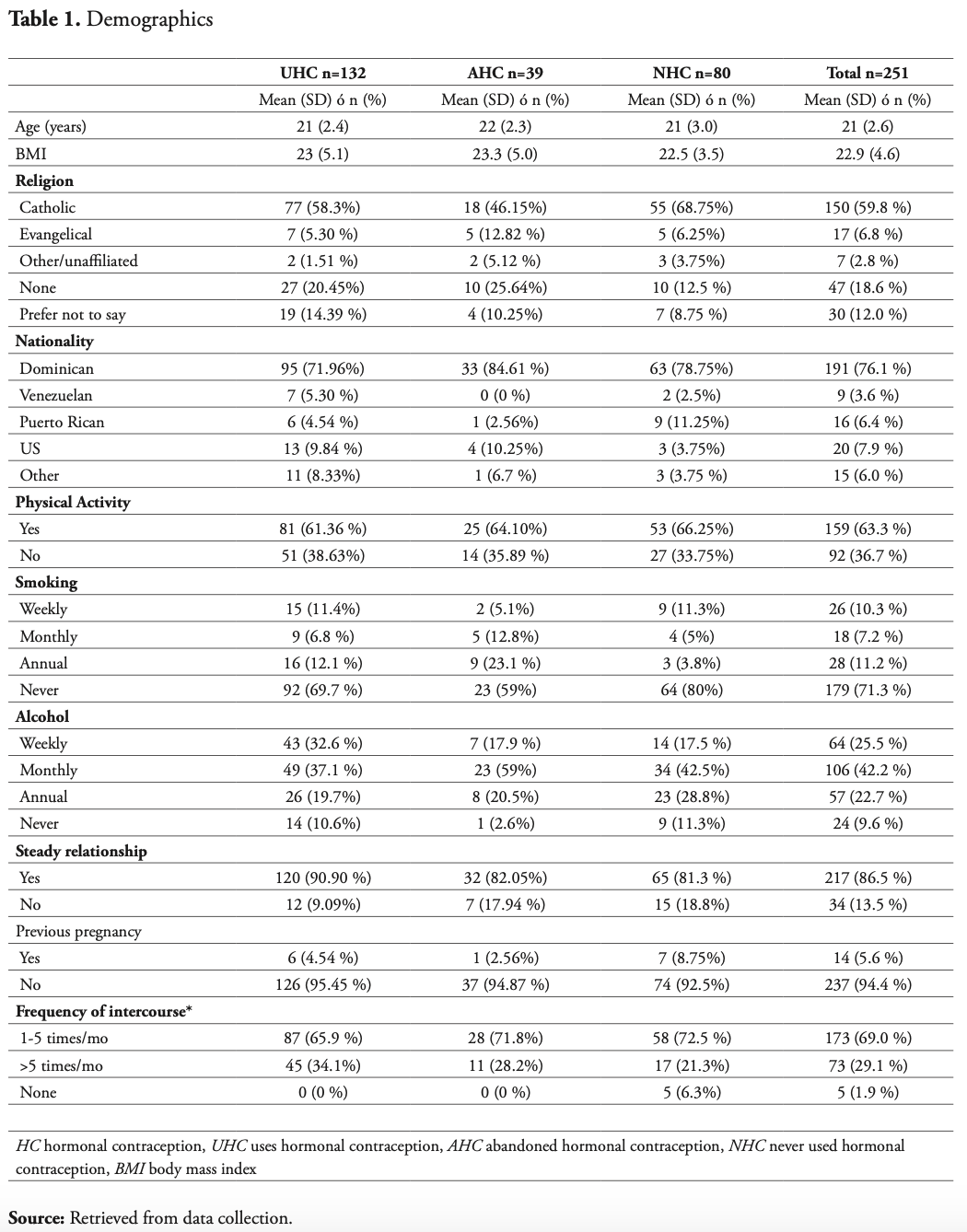
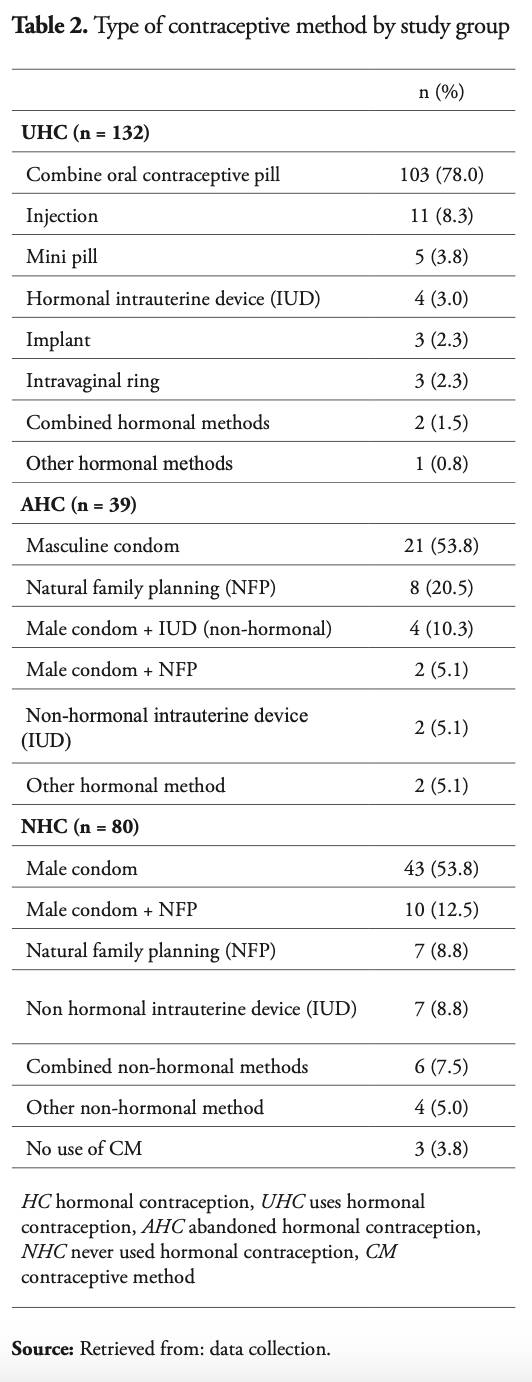
A total of 707 responses were received out of 2,270 online questionnaires that were distributed. Of these, 360 responses were eliminated by the exclusion criteria, while an additional 93 responses were eliminated due to inconsistency patterns, resulting in a total sample of 251 participants, representing 11.1% of the total female student body population. Table 1 summarizes the demographic findings of each study group. The total sample was similar in age, nationality, body mass index (BMI) and religion. A total of 86.5% of the study sample was in a stable relationship. The UHC group was the most sexually active. Table 2 summarizes the types of CM used by each study group. The most common forms of contraception were oral contraceptive pills (OCP) and male condoms. Overall, 52.6% of the total study population used HC.
3.2 Sexual function
3.3 Female sexual dysfunction (FSD)
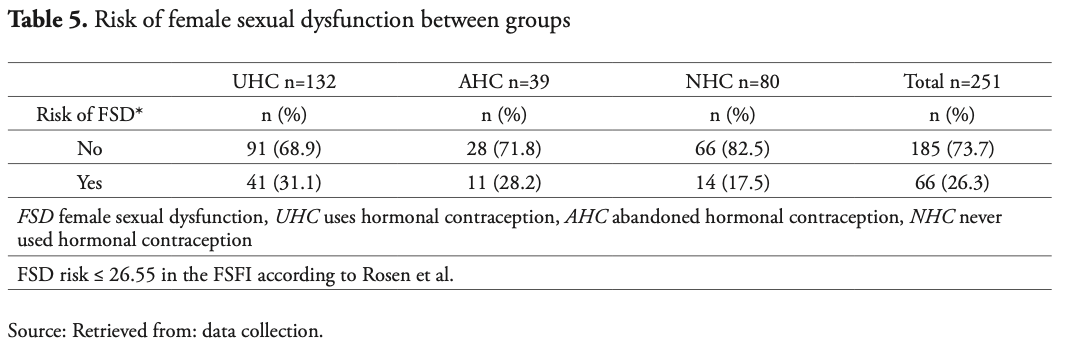
The FSFI indicates that any score equal to or under 26.55 suggests a risk of FSD, which is greater with a lower score11. The percentage of participants at risk of FSD in the NHC group was 17.5%, see Table 5. In contrast, the AHC and UHC groups presented a 10.7% and 13.5% increase in their population at risk of FSD, respectively, in comparison to those who had never used HC (NHC). Spearman’s correlation showed a weak, albeit statistically significant correlation between these differences (rho = 0.132; p = 0.037). Overall, 26.3% of the studied population presented a risk of FSD.
The study found that 43.0% of the population who abandoned HC (AHC) stated a negative impact on their FSF as the cause, almost half of which stated a specific impact on their sexual desire. Other causes of abandonment of HC were decreased lubrication and difficulty reaching orgasm. When asked if they felt their CM affected their FSF, 5% of the NHC group answered “YES, for worse”. This was about three and four-fold higher in the UHC and AHC groups, respectively (x2 = 0.018).
3.4 Satisfaction with CM
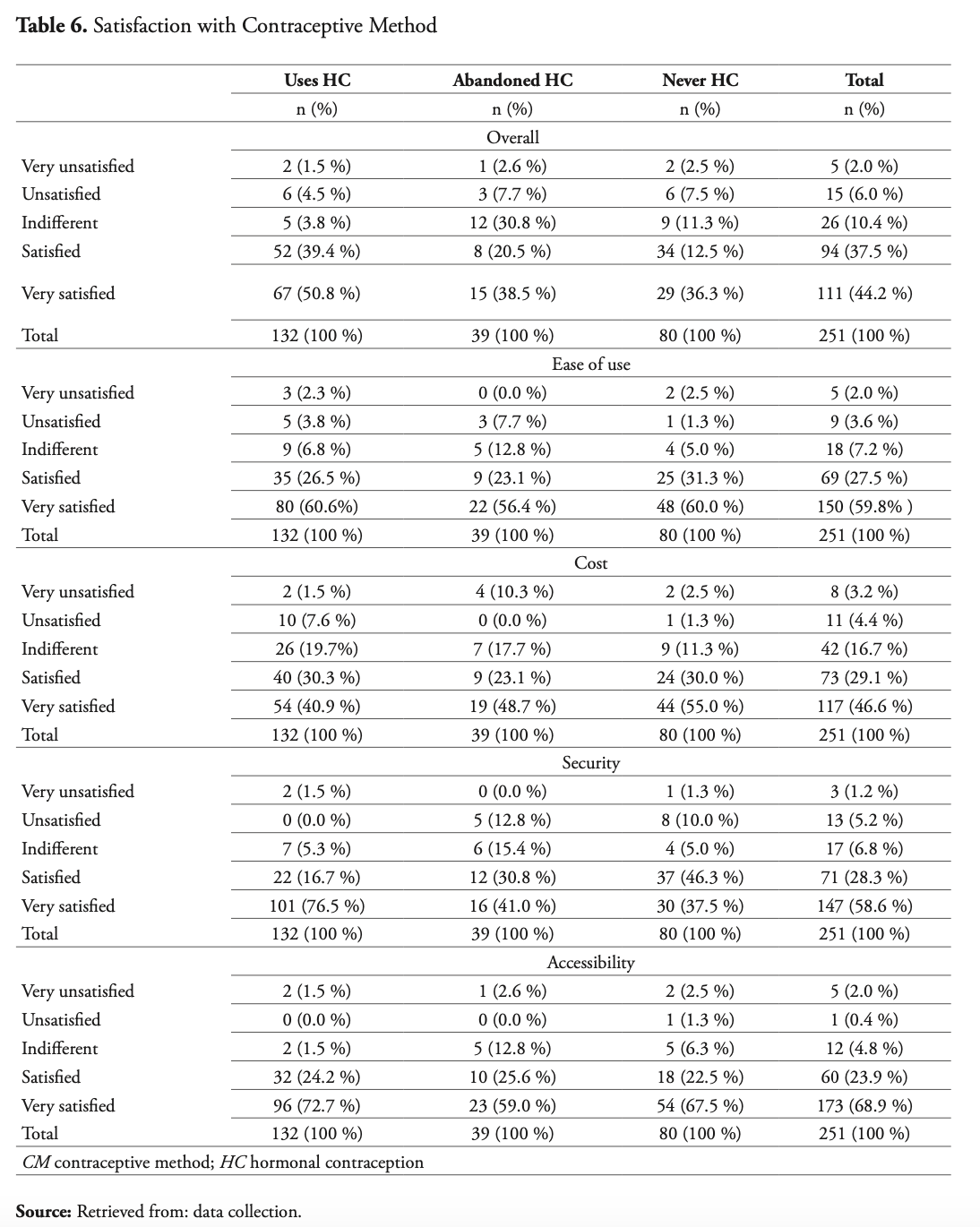
This item was evaluated in five aspects: overall, security, ease of use, accessibility, and cost; see Table 7. Current users of HC (UHC) reported the highest percentages of satisfaction in the categories of security, accessibility, and overall. In addition, a high level of satisfaction was reported throughout all groups for ease of use. Finally, the NHC group reported the highest satisfaction cost-wise.
3.5 Adherence to contraceptive method
When asked about the probability of abandoning their CM if it were to negatively affect their FSF, 65% of the entire population responded “likely” and “very likely”. As mentioned earlier, this was the main reason for abandonment in the AHC group.
4. Discussion
Evaluating the data obtained from this study and putting them into the context of previous findings on the matter4, 6, 13, similar results were found in the present study population. As hypothesized, the use of HC resulted in a lower FSFI score, and higher FSD risk in those currently using HC than in those who did not use HC, which suggests a direct relationship. The full knowledge of possible side effects from the use of HC should be available to patients in counseling to create an individualized and informed choice of CM that can better support sexual well-being and adherence to the method.
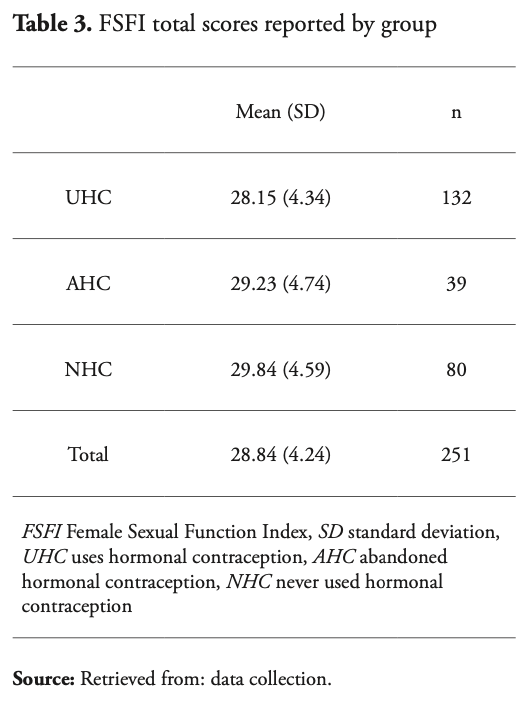
With the goal of evaluating the possible effects of HC on the FSF after its discontinuation, FSFI scores were compared between the NHC and AHC groups. These groups represent the non-current users of HC, in which the difference between them was the history of HC use. Results were also congruent with previous studies1, 4, 5, 8, 13: there was a statistically significant lower score in the AHC group. These findings suggest that the use of HC negatively impacts FSF and that there is a long-term effect of HC use on the FSF even after its discontinuation.
The study found a strong perception of decreased sexual function for the groups related to HC (UHC, AHC) in comparison to those who had not used HC (NHC), which was consistent with what Malmborg et al. had found in a similar study4. Results also showcased that despite a lower FSFI score and higher RFSD, users of hormonal contraceptives had high levels of satisfaction with their contraceptive method, particularly regarding the aspect of safety. This could suggest that for this specific population, given factors such as age, socioeconomic and educational background, contraceptive safety renders more importance than sexual well-being. With the aim of continuing to improve the sexual health and well-being of HC users, it is relevant to continue investigating the options of available contraceptives for women of reproductive age and their impact on female sexual health.
The results of this investigation on the effect of HC on FSF, the perception of its users and their willingness to abandon the method if their FSF is affected by it, demonstrate the clinical importance of being aware of the sexual side effects of the use of HC and the poor compliance it could render when counseling patients on birth control. This is particularly important in the Dominican Republic, where unwanted pregnancy rates are among the highest in Latin America and the Caribbean9, notably among students. Every year, 74 million women of low- and middle-income countries experience unplanned pregnancies, often resulting in increased economic burdens and the deterioration of their economic standing, lower rates of educational attainment, lower employment capacity, 25 million annual unsafe abortions, and 47 million annual maternal deaths14, 15.
It is important to note the study limitations. First, with limited financial resources, the study was unable to measure levels of testosterone and sex hormone-binding globulin (SHBG) between the study groups to further understand the differences in FSF interactions with HC. Second, given that the Dominican Republic is a highly socioeconomically heterogeneous society, these results cannot be generalized to the entire country’s population since this study included a narrow study population (students at a private university in the capital city) for which further studies will be necessary. Third, given that the study explored the effects of HC as a whole on the sexual function of its users, there was no distinction made between the type of contraceptives, compositions, dosages or route of administration. Any internal differences these could have on the effect of HC on sexual function was outside the scope of this study. Finally, given that data collection began during national lockdown due to COVID-19, the study allowed answers from participants’ most recent experiences, instead of the 4-week margin that the FSFI test is designed for, which may have resulted in recall bias.
In conclusion, this study shows an association between HC use and the increased risk of FSD in the context of female students of the Universidad Iberoamericana (UNIBE) between 18 and 30 years of age. In terms of the measurement of FSF impact by HC (tables 3 and 5), the findings in the AHC group, despite being lower than in the group of users (UHC), were consistently higher than in the NHC group, suggesting a possible long-term effect of HC use after its abandonment. Moreover, we found that negative HC impact on FSF was both a strong predictor and cause of abandonment of the contraceptive method in this population.
However, since the multifactorial etiology of female sexual dysfunction is more complex than this study can encompass, we cannot affirm a direct and causal relationship between the use of hormonal contraceptives and female sexual dysfunction. We can only confirm that in our study population, users of HC presented lower levels of FSF. More data is needed worldwide to continue to study this relationship.
Acknowledgements: The authors would like to thank Dr. Helena Chapman for providing editorial feedback on this article.
Referencias
- Both S, Lew-Starowicz M, Luria M, Sartorius G, Maseroli E, Tripodi F, et al. Hormonal contraception and female sexuality: position statements from the European Society of Sexual Medicine (ESSM). The Journal of sexual medicine 2019;16(11):1681-95. https://doi.org/10.1016/j.jsxm.2019.08.005
- United Nations, Department of Economic and Social Affairs, Population Division. Contraceptive Use by Method 2019: Data Booklet; 2019.
- Strufaldi R, Pompei LM, Steiner ML, Cunha EP, Ferreira JA, Peixoto S, et al. Effects of two combined hormonal contraceptives with the same composition and different doses on female sexual function and plasma androgen levels. Contraception. 2010;82(2):147-54. https://doi.org/10.1016/j.contraception.2010.02.016
- Malmborg A, Persson E, Brynhildsen J, Hammar M. Hormonal contraception and sexual desire: A questionnaire-based study of young Swedish women. The European Journal of Contraception & Reproductive Health Care. 2016;21(2):158-67. https://doi.org/10.3109/13625187.2015.1079609
- Wallwiener M, Wallwiener LM, Seeger H, Mueck AO, Zipfel S, Bitzer J, et al. Effects of sex hormones in oral contraceptives on the female sexual function score: a study in German female medical students. Contraception. 2010;82(2):155-9. https://doi.org/10.1016/j.contraception.2009.12.022
- Wallwiener CW, Wallwiener LM, Seeger H, Schönfisch B, Mueck AO, Bitzer J, et al. Are hormonal components of oral contraceptives associated with impaired female sexual function? A questionnaire-based online survey of medical students in Germany, Austria, and Switzerland. Archives of Gynecology and Obstetrics. 2015;292(4):883-90. https://doi.org/10.1007/s00404-015-3726-x
- Sanders SA, Graham CA, Bass JL, Bancroft J. A. Prospective study of the effects of oral contraceptives on sexuality and well-being and their relationship to discontinuation. Contraception. 2001;64(1):51-8. https://doi.org/10.1016/S0010-7
824(01)00218-9 - de Castro Coelho F, Barros C. The potential of hormonal contraception to influence female sexuality. International journal of reproductive medicine 2019; 2019. https://doi.org/10.1155/201
9/9701384 - Pan American Health Organization/World Health Organization. Core Indicators, https://opendata.paho.org/en/core-indicators; 2021 [accessed 13 July 2020].
- Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). Journal of medical Internet research. 2004;6(3):e132. https://doi.org/
10.2196/jmir.6.3.e34 - Sánchez-Sánchez B, Navarro-Brazález B, Arranz-Martín B, Sánchez-Méndez Ó, de la Rosa-Díaz I, Torres-Lacomba M. The female sexual function index: Transculturally adaptation and psychometric validation in Spanish women. International Journal of environmental research and public health. 2020;17(3):994. https://doi.org/10.3390/ijerph17030994
- Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. Journal of sex & marital therapy. 2000;26(2):191-208. https://doi.org/10.1080/009262300278597
- Panzer C, Wise S, Fantini G, Kang D, Munarriz R, Guay A, et al. Impact of oral contraceptives on sex hormone-binding globulin and androgen levels: a retrospective study in women with sexual dysfunction. The journal of sexual medicine. 2006;
3(1):104-13. https://doi.org/10.1111/j.1743-6109.
2005.00198.x - World Health Organization. The World Health Report 2005: make every mother and child count, https://www.who.int/publications/i/item/9241
562900; 2005 [accessed 29 May 2020]. - World Health Organization. High rates of unintended pregnancies linked to gaps in family planning services: New WHO study, https://www.
who.int/news/item/25-10-2019-high-rates-of-unintended-pregnancies-linked-to-gaps-in-family-planning-services-new-who-study. 2019 [accessed 9 February 2022].

