Ciencia y Salud, Vol. VI, No. 1, enero-abril, 2022 • ISSN (impreso): 2613-8816 • ISSN (en línea): 2613-8824 • Sitio web: https://revistas.intec.edu.do/
USE OF SIROLIMUS AND SCLEROTHERAPY FOR LYMPHATIC MALFORMATIONS IN A DEVELOPING COUNTRY: A CASE SERIES
Uso de sirolimus y escleroterapia para malformaciones linfáticas en un país en vías de desarrollo: una serie de casos
Cómo citar: Mena Canto R, Calderón M, Familia C. Uso de sirolimus y escleroterapia para malformaciones linfáticas en un país en vías de desarrollo: una serie de casos. cysa [Internet]. [citado 22 de febrero de 2022];6(1):81-5. Disponible en: https://revistas.intec.edu.do/index.php/cisa/article/view/2401.
Introduction
A lymphatic malformation (LM) is an anomaly that results from an error in the embryonic development of the lymphatic system and can be classified as macrocystic, microcystic, and mixed1,2. If acquired, lesions generally arise from obstruction of the lymphatic system due to trauma or infection3,4. Most of the lesions are congenital and develop in infants and children under 2 years of age5. The incidence of LM is estimated to be 1 per 6000-16,000 live births, with the majority of LMs (50-65%) evident at birth6. Two-thirds of all the reported cases are located in the head and neck3. Complications can include obstruction or distortion of vital structures, infection, bleeding, and pain7,8.
Case presentations
Patient 1
A 10-year-old girl visited a new primary care physician in January 2015 with a previous diagnosis of facial hemangioma, treated with propranolol for 3 years and no major change observed. Since there was no improvement with the treatment given, her parents decided to look for a second opinion. The patient had already done a sagittal MRI (T1 sequence, with and without contrast), coronal (T2 sequence) and axial (FLAIR). A consultation, through telemedicine, with the Cincinnati Children’s Hospital Medical Center was done and the definitive diagnosis was a lymphatic malformation. The therapy with sirolimus started in April 2015 along with trimethoprim/sulfamethoxazole.
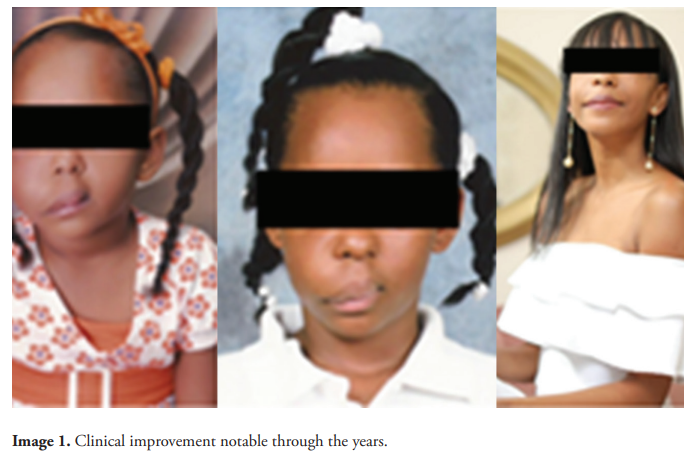
The patient was clinically better in follow up visits but in December 2015, the mass was more inflamed, which was the reason why an injection with bleomycin was appropriate. In July 2016, due to bleomycin unavailability, an injection with doxycycline was another option. In September 2016, a second injection with bleomycin was required. In December 2016, a third injection was applied. She completed 2 years of sirolimus therapy. The clinical Improvement was notable in subsequent visits [image 1].
Patient 2
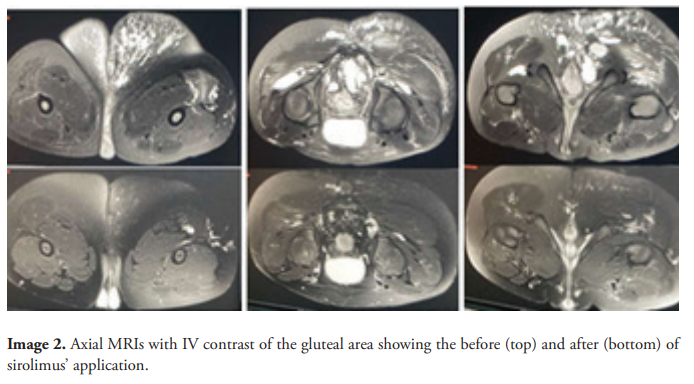
A previously healthy 8-year-old boy visited a new pediatrician in February 2017, complaining about a mass in his gluteal region. His physical exam revealed what appeared to be a vascular malformation that was also infected. An axial, sagittal and coronal MRI of the gluteal area (T1, T2 and fat sat sequences with gadolinium) was performed and a complete blood count, liver function tests, cholesterol, blood urea nitrogen, serum creatinine and uric acid were ordered. After the MRI, the diagnosis of lymphatic malformation with inflammatory changes due to infection was confirmed. Laboratory results showed a microcytic hypochromic anemia and a slightly reduced uric acid. The treatment decided was sirolimus for 24 months, trimethoprim/sulfamethoxazole and a supplementation with iron, folate and vitamin B12.
In the follow up visits, there was clinical evidence of improvement of the patient’s lymphatic malformation until the treatment with sirolimus was over. Then, in March 2019, an increase in the lesion’s volume was seen. Sirolimus was continued for another 24 months. In subsequent visits, the patient showed improvement. Different MRIs are attached in this report to compare the lesion before and after the sirolimus [image 2].
Patient 3
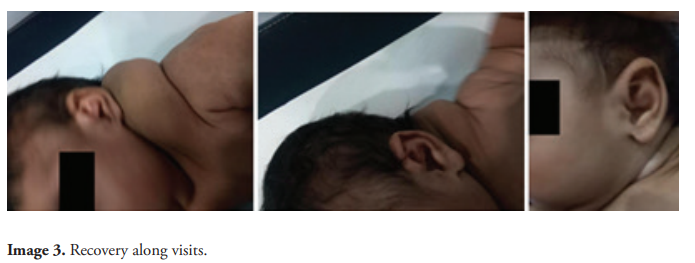
An otherwise healthy 7-day-old term girl visited her primary care physician in January 2019, with a mass in the left side of her neck. An MRI of the neck was performed with and without intravenous contrast administration. The findings consisted in a multiloculated cystic lesion. The diagnosis made was macrocystic lymphatic malformation. An injection with bleomycin was applied in February and March the same year. A remarkable improvement was evident in posterior visits [image 3].
Discussion
We describe three patients with diverse presentations of lymphatic malformations. These were evident at different points of life. Usually, an LM does not require any intervention, unless it is large or symptomatic1,9.
Sclerotherapy is first-line treatment for problematic macrocystic LM due to its superior efficacy and a lower complication rate shrinking the lesion and alleviating symptoms7,8. According to Kim et al.10, surgical removal of macrocystic LM is indicated if the lesion is symptomatic and sclerotherapy is not possible anymore. Resection can be curative if the lesion is small and well localized. Oral sirolimus can also be effective for diffuse problematic lesions11.
Among the sclerosing agents, the most commonly used are doxycycline, sodium tetradecyl sulfate, ethanol and bleomycin10. The improvement after the use of bleomycin and/or doxycycline, alone or as an add-on for the sirolimus, was noticeable in cases 1 and 3. Bleomycin and doxycycline are easily available, inexpensive and have well known effectiveness, which is convenient for a developing country12.
Sirolimus, used in patients 1 and 2, was efficacious and safe, a fact that goes along with the conclusions of Adams et al.13 The proper follow up was given (and it is still ongoing) to those children, with different blood analysis and images if needed. As with other experiences with that medication, we provide ours as supportive evidence14,15.
Referencias
- Greene AK, Perlyn CA, Alomari AI. Management of lymphatic malformations [Internet]. Clinics in Plastic Surgery. Clin Plast Surg, 2011;38:75–82. Available from: https://pubmed.ncbi.nlm.nih.gov/21095473/
- UpToDate. Diaz LZ. Vascular lesions in the newborn. [Online]. Available from: https://www.uptodate.com/contents/vascular-lesions-in-the-newborn?search=Vascular%20lesions%20in%20the%20newborn&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1 [Accessed 11 April 2021] .
- Brock ME, Smith RJH, Parey SE, Mobley DL. Lymphangioma. An otolaryngologic perspective. Int J Pediatr Otorhinolaryngol [Internet]. 1987;14(2–3):133–40. Available from: https://pubmed.ncbi.nlm.nih.gov/3436717/
- Aneeshkumar MK, Kale S, Kabbani M, David VC. Cystic lymphangioma in adults: Can trauma be the trigger? Eur Arch Oto-Rhino-Laryngology [Internet]. 2005 Apr;262(4):335–7. Available from: https://pubmed.ncbi.nlm.nih.gov/15841412/
- Bauman NM, Giguere CM, Manaligod JM, Sato Y, Burke DK, Smith RJ. Management of lymphatic malformations-If, when and how. Oper Tech Otolaryngol Head Neck Surg, 2002;13:85–92. Available from: https://doi.org/10.1053/otot.2002.31396
- Kindblom LG, Angervall L. Tumors of lymph vessels. Contemp Issues Surg Pathol, 1991; 18:163.
- Burrows PE, Mitri RK, Alomari A, Padua HM, Lord DJ, Sylvia MB, et al. Percutaneous sclerotherapy of lymphatic malformations with doxycycline. Lymphat Res Biol [Internet]. 2008;6(3–4):209–16. Available from: https://pubmed.ncbi.nlm.nih.gov/19093794/
- Chaudry G, Guevara CJ, Rialon KL, Kerr C, Mulliken JB, Greene AK, et al. Safety and Efficacy of Bleomycin Sclerotherapy for Microcystic Lymphatic Malformation. Cardiovasc Intervent Radiol [Internet]. 2014;37(6):1476–81. Available from: https://pubmed.ncbi.nlm.nih.gov/24938907/
- UpToDate. Greene AK, Sudduth CL. Overview of vascular intervention and surgery for vascular anomalies. [Online]. Available from: https://www.uptodate.com/contents/overview-of-vascular-intervention-and-surgery-for-vascular-anomalies?search=Overview%20of%20vascular%20intervention%20and%20surgery%20for%20vascular%20anomalies&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1 [Accessed 11 April 2021].
- Kim SW, Kavanagh K, Orbach DB, Alomari AI, Mulliken JB, Rahbar R. Long-term outcome of radiofrequency ablation for intraoral microcystic lymphatic malformation. Arch Otolaryngol - Head Neck Surg [Internet]. 2011;137(12):1247–50. Available from: https://pubmed.ncbi.nlm.nih.gov/22183906/
- Wiegand S, Wichmann G, Dietz A. Treatment of Lymphatic Malformations with the mTOR Inhibitor Sirolimus: A Systematic Review [Internet]. Lymphatic Research and Biology. Mary Ann Liebert Inc, 2018;16:330–9. Available from: https://pubmed.ncbi.nlm.nih.gov/29924669/
- Vlahovic A, Gazikalovic A, Adjic O. Bleomycin sclerotherapy for lymphatic malformation after unsuccessful surgical excision: case report. Acta Otorhinolaryngol Ital [Internet]. 2015;35(5): 365-7. Available from: https://europepmc.org/articles/PMC4720922
- Adams DM, Trenor CC, Hammill AM, Vinks AA, Patel MN, Chaudry G, et al. Efficacy and Safety of Sirolimus in the Treatment of Complicated Vascular Anomalies. Pediatrics, 2016;137(2):e20153257. Available from: https://doi.org/10.1542/peds.2015-3257
- Vlahovic AM, Vlahovic NS, Haxhija EQ. Sirolimus for the Treatment of a Massive Capillary-Lymphatico-Venous Malformation: A Case Report. Pediatrics, 2015;136(2):e513 LP-e516. Available from: https://doi.org/10.1542/peds.2014-3469
- Hammill AM, Wentzel M, Gupta A, Nelson S, Lucky A, Elluru R, et al. Sirolimus for the treatment of complicated vascular anomalies in children. Pediatr Blood Cancer [Internet]. 2011;57(6):1018–24. Available from: https://pubmed.ncbi.nlm.nih.gov/21445948/

