Ciencia y Salud, Vol. V, No. 1, enero-abril, 2021 • ISSN (impreso): 2613-8816 • ISSN (en línea): 2613-8824 • Sitio web: https://revistas.intec.edu.do/
Sobredosis por bloqueadores de calcio en una mujer
CALCIUM CHANNEL BLOCKER OVERDOSE IN A FEMALE PATIENT
Cómo citar: Veras Victoria A, Mejia de la Cruz DM, Mateo de la Cruz MB, Roedan Oliver F, Henriquez Perez PM. Calcium channel blocker overdose in a female patient. cysa [Internet]. 15 de febrero de 2021 [citado 23 de febrero de 2021];5(1):109-16. Disponible en: https://revistas.intec.edu.do/index.php/cisa/article/view/2056
Background
Calcium channel blockers are a family of medication used for hypertension, atrial fibrillation, chest angina, subarachnoid hemorrhage1. Although uncommon, due to its many uses, intoxication, and even overdose can happen and lead to a rapid hemodynamic collapse for the patient2. More than one-third of deaths from cardiovascular drug overdose is related to CCBs3.
Here we present the case of a young female asthmatic patient who overdosed with 53 tablets of nifedipine of 10 mg each, needing ventilator support as well as vasopressor support. Given the low number of case reports on the subject and lack of consensus on adequate treatment4, we decided to publish how the patient was managed.
Timeline
19-year-old female patient with a past medical history of suicide attempt by overdose with a second-generation antihistaminic (loratadine) 3 years ago, and asthma treated with inhaled hydrocortisone, albuterol and salmeterol is brought to the emergency department of the Hospital General Plaza de la Salud for presenting episodes of emesis at her home when she ingests solid and liquid foods. The patient had previously ingested 53 tablets of nifedipine 10 mg the previous day and had a gastric lavage done at another center afterward. She has referred to a psychiatrist afterward where an unspecified medication was prescribed to which the patient presented poor adherence.
At the moment of evaluation, the patient was conscious, hypoactive, looking acutely ill hypotensive with a systolic pressure of 80 mmHg and a diastolic pressure of 20 mmHg, which led to the administration of calcium gluconate, her blood pressure raised to 108/74 mmHg, heart rate of 79 beats per minute, respiratory rate of 18 respirations per minute, and oxygen saturation of 100%. The rest of the examination was remarkable. A decision was made to keep the patient for observation at the emergency.
In the meantime, she became hypotensive again and the Cardiovascular ICU unit was consulted where the decision was made for the patient to be admitted to the cardiovascular ICU.
Diagnostic procedures:
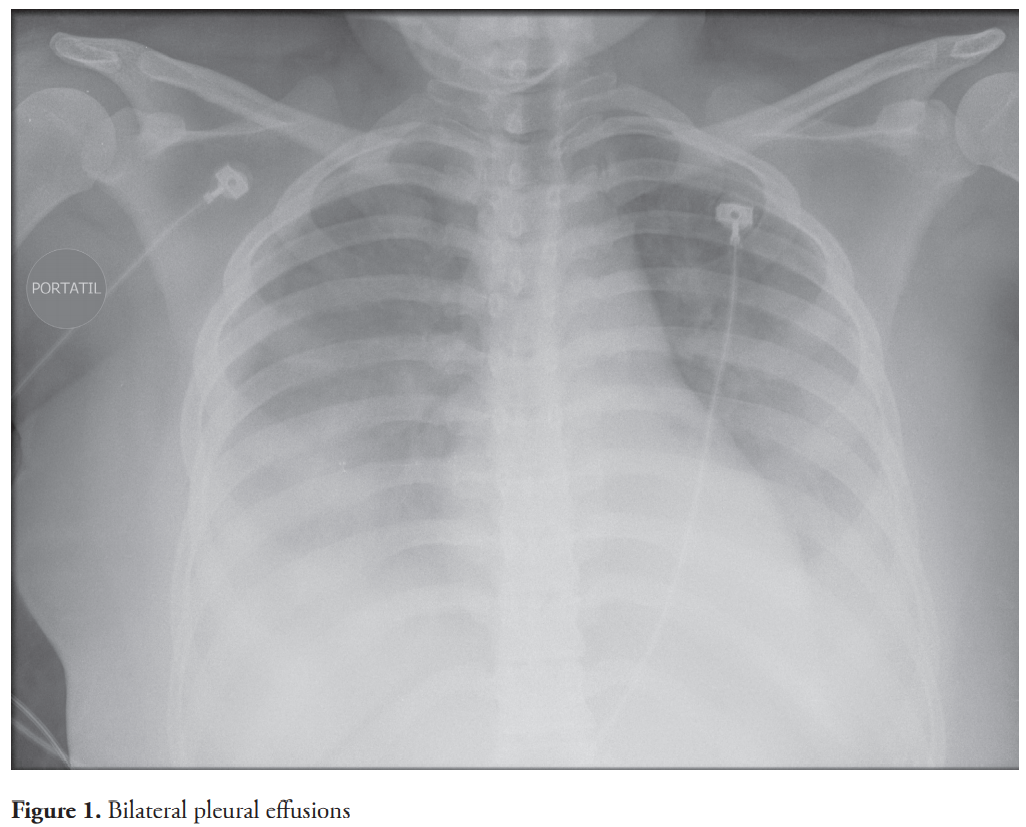
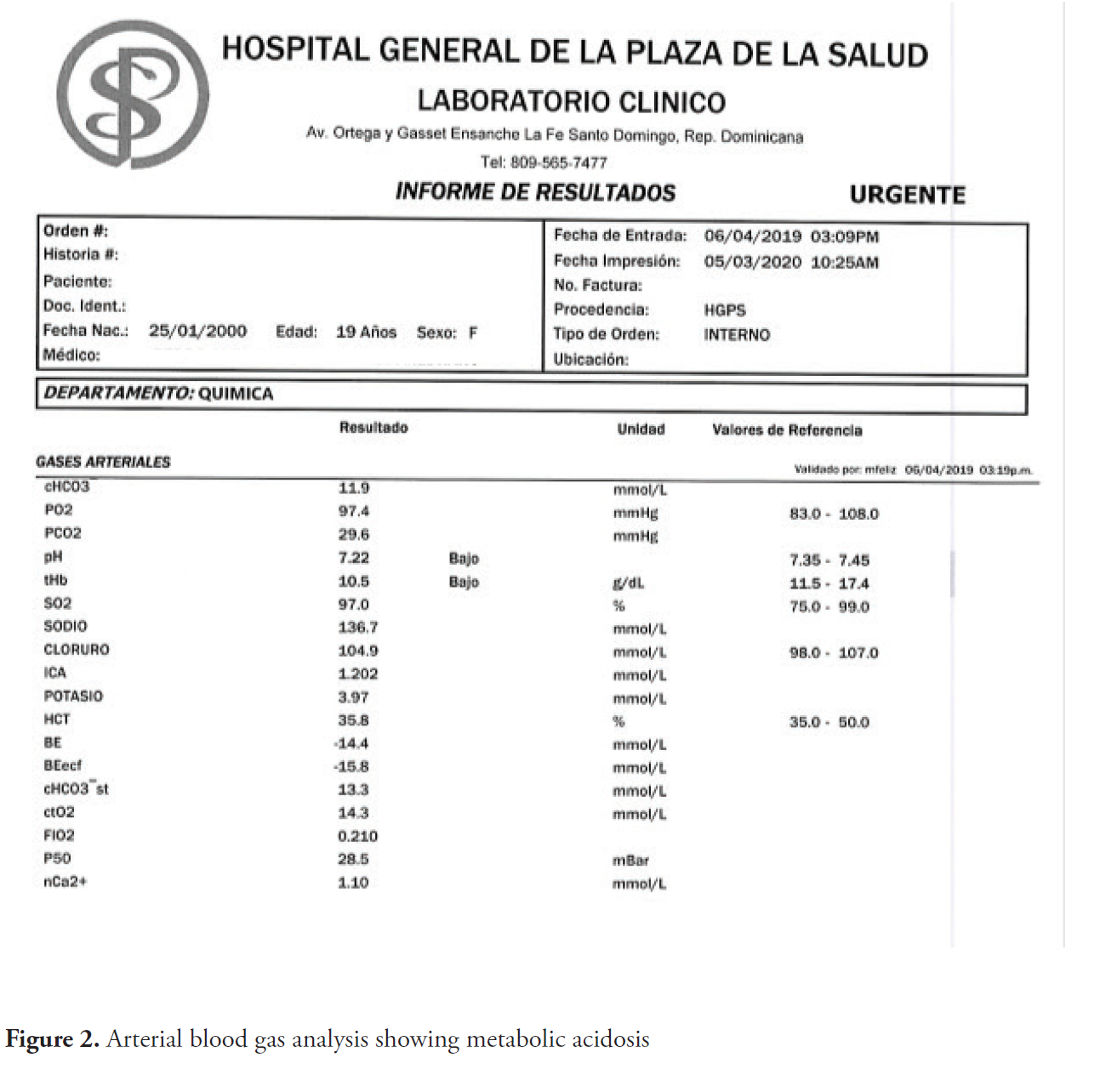
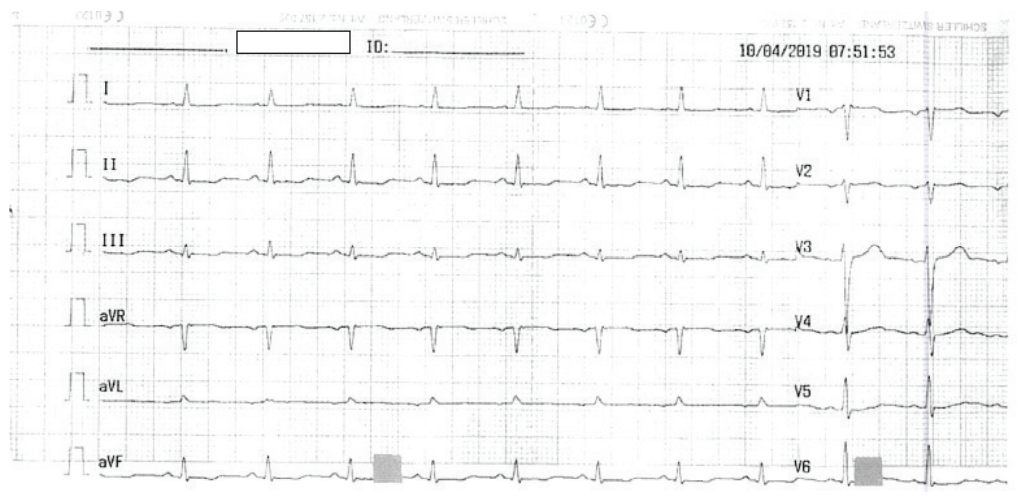
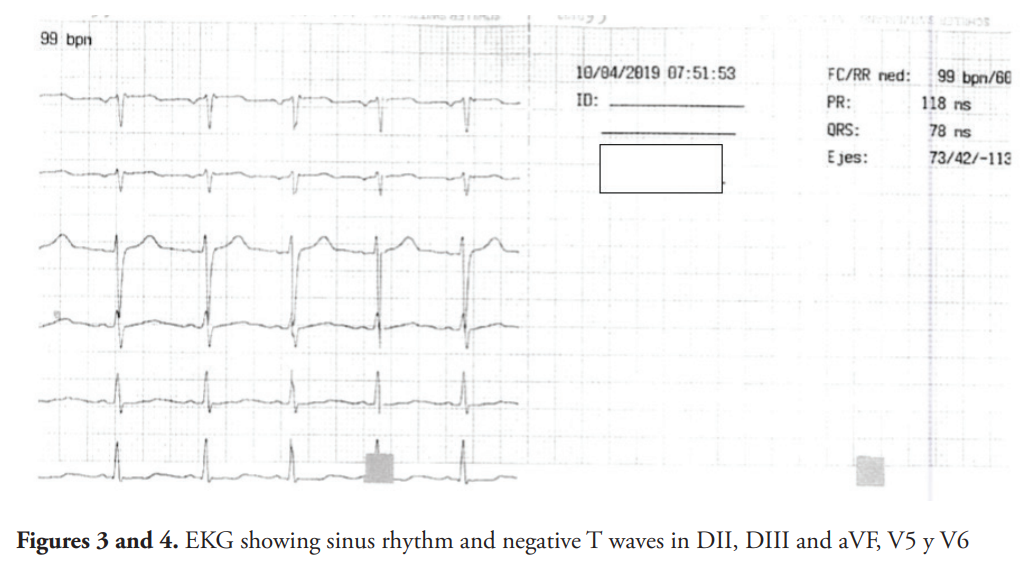
A chest X-ray showed bilateral pleural effusions (Figure 1). Transthoracic echocardiogram showed no abnormalities with an ejection fraction of 80%. Abdominal sonography showed results within normal parameters. Among the laboratory tests performed, pertinent positives were: ABG with pH: 7.33, PO2: 47.9, HCO3: 15.5, BUN: 27, WBC: 16.36, HTC: 29.3, Hg: 9.7 which then progressed to metabolic acidosis (Figure 2) with a pH: of 7.22, PCO2: 29.6, HCO3: 11.9. Electrocardiogram tracing evidenced sinus rhythm with a HR of 99 beats per minute and inversion of T waves in DII, DIII, aVF, V5, and V6 (Figure 3 and Figure 4).
Interventions:
At the moment of her admission, the patient was hypotensive, sedated, with a mixed acidosis. Due to her persistent hypotensive levels support with noradrenaline with continuous infusion of calcium chloride and the adrenaline was initiated. The patient also presented mixed metabolic acidosis and mean diastolic of 60 mmHg which led to intubation of the patient and placement of a central venous line for administration of inotropic and vasopressors.
A chest X-ray was done where it evidenced bilateral pleural effusions (Figure 1). The noradrenaline and pressor support was adjusted to the hemodynamics the patient presented, reaching a maximum dose of 0.18 mcg/kg/min for noradrenaline, with a posterior reduction on the second day of admission in the ICU and initiation of vasopressin 0.06 units/ min. Vasopressin and noradrenalin were removed on the 4th day of hospitalization. Furosemide 20 mg is indicated for the management of chest X-ray congestion.
On her second day in the ICU patient presented a rash on the face and upper chest, which led to the administration of hydrocortisone. The patient also presented abundant secretions on the tracheal tube with a BP of 115/52 mmHg and metabolic acidosis. During her admission at the ICU patient developed transvaginal bleeding, which after evaluation by the gynecology department a B-HCG hormone level was ordered that turned out negative. After correction of metabolic acidosis is done, the patient starts presenting an increase in WBC (16,000 mm3) and after consultation with the infectious diseases and the positive findings of crackles in the right lung led to the prescription of ceftriaxone 1 gr every 12 hours and clindamycin 600 mg every 8 hours, the treatment improved the WBC count of the patient. The patient was extubated on her 5th day of hospitalization without eventualities and was maintained on continuous oxygen through a face mask. On the 7th day of hospitalization, the patient is moved from ICU to the medical ward where she remained on observation for 4 days until discharge, after complete resolution of opacity on chest X-ray with a scheduled appointment with the psychiatric department.
Follow up:
Once the patient was authorized for discharge by all the involved parts in the case, psychiatric follow up scheduled as well as treatment based on psychotherapeutic intervention, making sure the patient preserved her self-preservation instinct.
Discussion
Nifedipine is the first calcium channel blocker from the dihydropyridine family. These have a vasodilator effect and they also increase coronary flow; it blocks the entrance of calcium into vascular smooth muscle cells2 5 6. It also decreases myocardial contractility6. Nifedipine is a molecule that works by decreasing systemic blood pressures, fundamentally by reducing systemic vascular resistance (SVR)7.
They are 3 different classes of clinically useful calcium channel antagonist; the members of each class bind to a different receptor site within the calcium channel7. These drugs primarily affect arterial resistance vessels, with only minimal effects on venous capacitance vessels8.
Nifedipine is fast-acting and almost completely absorbed after its oral administration (90%), although due to the first-pass metabolism in the liver, its bioavailability is reduced to 50-70%. After oral administration of the standard nifedipine formula, its hypotensive effects begin to manifest between 30 minutes and an hour, reaching its maximum effect between 30 minutes and 2 hours5. Presystemic metabolism of nifedipine results in inactive metabolites with half-live if about 9 hours9.
An overdose with this type of medication can cause a lot of side effects that can eventually lead to neurogenic syndrome and cardiovascular collapse4 10.
Calcium channel blockers reduce the entrance of calcium to the cardiac muscle and to the walls of the blood vessels; this allows blood to flow easily reducing the blood pressure11.
The patient in this case report presented intoxication with clinical manifestations proper of the medication such as hypotension, metabolic acidosis, cardiogenic shock, azotemia with a hemodynamic and clinical presentation like previously reported cases. It manifested initially as repeated emesis after ingestion of solid and liquid foods followed by hypotension with compensated tachycardia and bilateral pleural effusions and mixed acidosis that progressed to metabolic acidosis. The management included admission to the cardiovascular ICU, support with mechanical ventilation due to constant hypotension, and mixed metabolic acidosis. She was also managed with noradrenaline and pressor support due to her low-tension levels, reaching a maximum dose of 0.018 mcg/kg/min for noradrenaline and a maximum dose of 0.06 units for vasopressin, until being reduced and titrated until removed. The patient was also managed with 100 UI of regular insulin in an infusion of calcium twice during her admission to ICU. Insulin is described along with extracorporeal circulation as the strongest evidence, although it is low quality 2 4. Since calcium channel blockers reduce insulin secretion, creates tissue insulin resistance, and interfere with glucose catabolism leading to lactic academia and metabolic acidosis, hyperinsulinemic euglycemia (HIE) has emerged as a potent therapy for severe calcium channel blocker toxicity to reverse the instability caused by CCBs overdose 12 13. The potential toxicity of these agents is substantial and is often underappreciated by the public14. A consensus has not been reached on what could be used as an antidote for CCB overdose15.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributors
Veras, A.: History taking of patient, including past medical history. Gathering of part of the images from the medical record. Major contributor in the authorship, structure and proofreading of the article.
Mejía, D.: supervisor of the case report elaboration. A major contributor to the correct structure of the relevant information and images needed for the case report. Critic revision of the report.
Mateo, M.: contributor in the gathering of data from the patient after her discharge from the ICU as well as contributor to the discussion of the case and gathering of images.
Roedan, F.: contributor to the gathering and formatting of images for the case report. Contributor in the authorship and proofreading of the article.
Henríquez, P.: attending physician directly involved in the care of the patient during her stay in the Cardiovascular ICU. Critic revision of the report.
Declaration interest
None
Referencias
- University of Illinois. Nifedipine-oral-tablet [Internet]. Healthline. february14, 2017. Available from: https://www.healthline.com/health/nifedipine-oral-tablet
- Zegarra J. Meza M, Cornejo C, et al. Amlodipino y choque vasodilatado en una unidad de cuidados intensivos de un hospital general. Reporte de caso. RevMedHered. 2017 Jun;28(2):101–4.
- Olson KR, Erdman AR, Woolf AD, Scharman EJ, Christianson G, Caravati EM, Wax PM, Booze LL, Manoguerra AS, Keyes DC, Chyka PA, Troutman WG, American Association of Poison Control C. Calcium channel blocker ingestion: an evidence-based consensus guideline for out-of-hospital management. Clin Toxicol 2005; 43:797-822.
- Le Sage J, Poitras J, Provencher D N, Juurlink, Blais M, St-Onge P-A, Dubé S, Gosselin C, Guimont J, Godwin P M, Archambault J-M, Chauny A J, Frenette M, Darveau N. Treatment for calcium channel blocker poisoning: a systematic review. Pubmed. 2014 Oct 6;52(9):926– 44. Available from https://pubmed.ncbi.nlm.nih.gov/25283255/
- Rodríguez MO. Curso básico sobre hipertensión. Tema 5. Bloqueantes de los canales del calcio. elsevier farmacia profesional [Internet]. 2017 Sep;31(5):26–32. Available from: https://www.elsevier.es/es-revista-farmacia-profesional-3-articulo-curso-basico-sobre-hipertension-tema-X0213932417617164
- PubChem [Internet]. Bethesda (MD): National Library of Medicine (US), National Center for Biotechnology Information; 2004-. PubChem Compound Summary for CID 4485, Nifedipine; [cited 2021 Jan. 14]. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/Nifedipine
- Tellez-Mendez R, Curiel R, Marianela y Salcedo M. F. Nifedipina de liberación programada en micro-gránulos para el control de la enfermedad hipertensiva del embarazo. Rev ObstetGinecolVenez [online]. 2012;72(1):13–8.
- Klabunde RE. Cardiovascular Pharmacology Concepts [Internet]. www.cvphysiology.com, 2015. Available from: https://cvpharmacology.com/vasodilator/CCB
- Egan HHT. Pharmacology and Physiology for Anesthesia [Internet]. Elsevier; 2018. Available from: https://www.elsevier.com/books/pharmacology-and-physiology-for-anesthesia/hemmings/978-0-323-48110-6
- Aronson JK. Calcium channel blockers. In: Aronson JK, ed. Meyler’s Side Effects of Drugs. 16th ed. Waltham, MA: Elsevier; 2016:23-39
- Perin EC, Coulter S, Howard K, Schramm et al. Bloqueantescálcicos [Internet]. Texas Heart Institute. Available from: https://www.texasheart.org/heart-health/heart-information-center/topics/calcium-channel-blockers/
- Chakraborty RK, Hamilton. RJ. Calcium Channel Blocker Toxicity. S, editor. Treasure Island (FL): StatPearls [Internet]; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537147/ (accessed on June 10, 2020).
- Nickson C. Calcium Channel Blocker Toxicity [Internet]. LITFL-Life-in-the-FastLane-760-180. 2020. Available from: https://litfl.com/calcium-channel-blocker-toxicity/´
- Traub SJ, Grayzel J, editor. Calcium channel blocker poisoning. uptodate; 2020.Available from https://www.uptodate.com/contents/calcium-channel-blocker-poisoning#H22
- Murphy BNG. Calcium Channel Blocker Toxicity [Internet]. The California Poison Control System. 2005. Available from: https://calpoison.org/news/calcium-channel-blocker-toxicity

